Early Postpartum Tips for Pelvic Floor
Women’s health expert Physiotherapist Jenny Devlin gives insight on what you might expect from your postpartum body and the best approach to begin exercise and optimise your recovery
WRITTEN BY JENNY DEVLIN, MSK PHYSIOTHERAPIST AND SPECIALIST WOMEN’S HEALTH PHYSIOTHERAPIST AT PHYSIO EFFECT
So, you’ve just had a baby… CONGRATULATIONS!!
The first days and weeks postpartum can be a blur and prioritizing pelvic floor exercises might not be at the forefront of everyone’s mind. There are some things you can do, however, throughout the day to start working on your pelvic floor while also enjoying sweet baby cuddles.
BREATHE
Something that we do every day but often don’t do well. Once we have had a baby our breathing is often altered as our baby has been taking up the space in our abdominal cavity and achieving a deep breath might have been tricky for the past few months. Remembering how to take deep breaths can help with the healing process. Our diaphragm and pelvic floor move together and as a result breathing deeply in can help relax and lengthen the pelvic floor muscles and conversely exhaling can help engage the same muscles.
Getting the muscle pump of the pelvic floor working can aid pelvic congestion and help heal the tissues through lymphatic drainage.
Deep breathing can also help us enter into ‘rest and digest’ mode which can help us feel calm and decrease anxiety and enjoy being present with our baby.
You can practice breathing anywhere but it might be easiest sitting or in a semi-reclined position. Make sure you’re comfortable. Inhale slowly through the nose, feeling the air fill the lungs and the pelvic floor lengthen. Exhale gently through the mouth and feel the recoil of the tissues. Keep your shoulders and jaw relaxed. You can learn more about the structures that make up your abdominal cannister, including your pelvic floor in our recent Blog Post.
Posture
Throughout the day, check in with your posture while sitting, standing and moving around. Has your posture changed since having your baby? Can you find your way back to your previous position?
How we hold ourselves while feeding baby for many hours per day is important. Make sure baby is supported to come up to you, so that you don’t have to hunch over to feed. Try to maintain an upright posture for feeding as much as you can - it has an impact, not only on your back, neck and shoulders, but on your pelvic floor too! This NHS guide has ideas alternative breastfeeding positions from the commonly adopted ‘Cradle Hold.’
Have a think when you’re holding baby, are you always holding them on one side? Can you switch? Can you wear them for a while in a carrier instead of carrying them? Try placing your hands on your ribs and stacking them over your pelvis.
There are lots of little ways we can improve postures throughout the day to make our pelvic floor a little happier and function better too!
Pelvic Floor Exercises
Throughout the day try to practice a few pelvic floor muscle contractions. You may find it easier to do it lying down or in sitting. Check in with yourself and see what you can feel. You should be able to feel a gentle lift of the pelvic floor without your pelvis tilting and without your legs or bum muscles working hard. You should also be able to feel it relaxing. Try for some longer contractions and some short, fast ones too.
Women’s health Physiotherapist Mariam Kilpatrick demonstrating the ‘Butterfly’ Technique to connect with your pelvic floor.
Gentle Exercise
In the first days postpartum, take it easy. No matter how your baby was born, the body goes through a lot to bring your little one into the world. You might feel like you can do more exercise wise, but do you really need to? Give your body time to rest and recover and gradually build in your exercises. The first days or weeks might start out just thinking about pelvic floor, core and posture and progress from there. We are all about getting you back to doing the things you LOVE so let’s make sure you’re doing them sequentially in a way that’s right for your body and will allow you to continue doing them long term!
See a Pelvic Floor Physiotherapist
Pelvic floor symptoms are common, but they are not normal! We hear a lot of people normalizing pain or incontinence. Often ladies don’t know there is help out there but there is level 1, grade A evidence to show that pelvic floor assessment and treatment can improve pelvic floor function. Enjoy baby cuddles and gentle progressive exercises and anywhere from the 6 week mark, come and see us and have a pelvic floor evaluation so we can do an assessment, assist with any symptoms and help you work towards your goals, no matter what they are.
Pelvic Organ Prolapse
Pelvic Organ Prolapse - Signs, Symptoms and Treatment
PELVIC ORGAN PROLAPSE
WRITTEN BY JENNY DEVLIN, MSK PHYSIOTHERAPIST AND SPECIALIST WOMEN’S HEALTH PHYSIOTHERAPIST AT PHYSIO EFFECT. MCSP & HCPC
For a lot of people a diagnosis of, or even the thought of, pelvic organ prolapse is terrifying. It is extremely common though with the Royal College of Obstetricians & Gynaecologists suggesting that as many as 1 in 10 women over the age of 50 are affected. This number may well be higher with an increasing risk of complications after pregnancy and childbirth.
The good news is that many people are able to reduce or resolve their prolapse with the help of a pelvic floor physiotherapist. In this blog we explain more about Pelvic organ prolapse and look at how our experienced and specially trained Pelvic health Physiotherapists can help you.
What is pelvic organ prolapse (POP)?
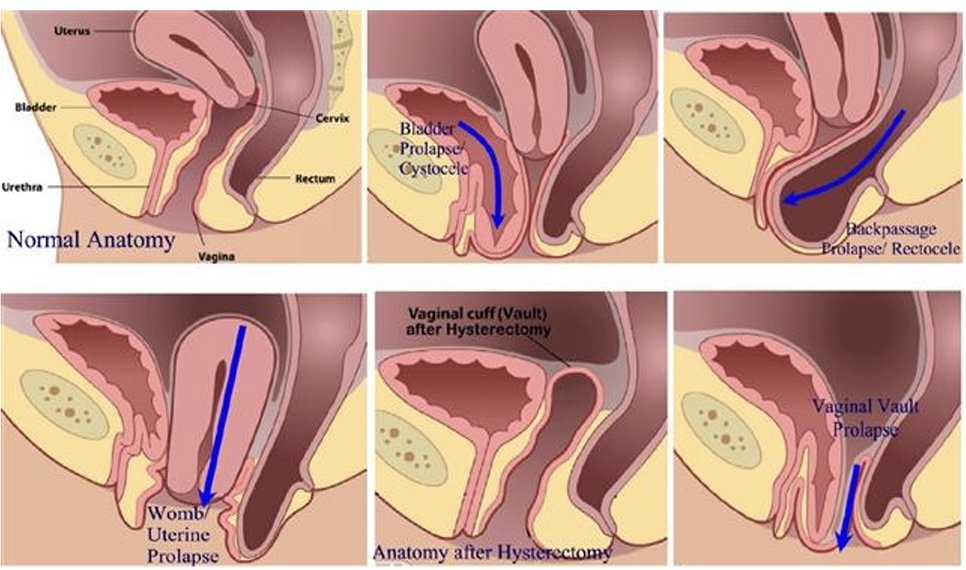
A pelvic organ prolapse occurs when a pelvic organ (or organs) bulge into the vaginal space. Strained, tight or weak muscles, ligaments or fascia can contribute to this. It can occur in different ways and we name the POP based on the organ that is not in its optimal position. A bladder prolapse (or cystocele) is where the bladder pushes against the front wall of the vagina. A uterine prolapse is where the uterus drops down into the middle of the vaginal space and a rectocele is when the rectum moves into the space at the back of the vaginal canal. You can also have a vaginal vault prolapse which occurs after a hysterectomy.
Pelvic Organ Prolapse
Symptoms of a pelvic organ prolapse
Prolapse affects everyone in a very unique way both physically and mentally. Some people live with prolapse and do not experience any symptoms. Other people can experience any number of symptoms which can be mild or affect your quality of life. Symptoms include:
pressure or heaviness in your pelvis area, which is often worse at the end of the day or with exercise
low back pain
urinary symptoms such as a slower stream, increased frequency or urgency to void, feeling of incomplete emptying of the bladder, urinary incontinence
bowel problems such as constipation, straining, feeling like the bowel doesn’t empty completely, increased frequency of bowel movements, faecal smearing (stool on the tissue after wiping clean), incontinence of faeces
Discomfort during sexual intercourse
Treatment options for pelvic organ prolapse
Pelvic Health Physiotherapy Assessment
Great news! Pelvic floor physiotherapy may be able to help with your symptoms of POP. Our team can help suggest changes you can make to your day to day routine to manage pressure on the organs, help with toilet positions to aid more effective urination/defecation.
Our specially trained Physiotherapists can assess muscle tension in the pelvic floor and abdominal muscles and help you to release this. We can also assess the strength and endurance of the muscles and teach you how to improve this if need be.
Physio instructed strengthening
We can guide you on correct strength and endurance exercises to help support the pelvic organs and the pelvis itself. This can help you in everyday functions when straining or lifting and on safely returning to sport. We can also make individual suggestions for more comfortable positions for intercourse.
Pessary For Pelvic Organ Prolapse
At Physio Effect our specialist team can assess and fit a pessary. A pessary is a device you wear inside the vagina, intermittently or continuously, to help hold things in position while you do the things you love. Once it is in place, you don’t feel anything but it can provide instant relief from that heaviness or pressure and can help with symptoms of incontinence too.
Cube Pessaries
Best of all once fitted these pessaries are designed for self management so you are in complete control and can remove and fit the pessary as required. After assessment and discussing your individual symptoms and needs our physiotherapists can help you decide if surgery might be the best route for you if conservative therapy has not worked.
We are here to help so please ask us anything. Hopefully this information makes things seem a bit less overwhelming and gives you hope that your symptoms can be improved. Give us a call or book in online for a full assessment and personalised treatment plan.