Pain - Finding Relief & Taking Control
That ache in your back, the stiffness in your neck, the twinge in your knee – these are common experiences we all face from time to time. Pain is something we will all have to manage at some point in our lives. Your understanding and response to pain is crucial in optimally managing & ultimately reducing you pain
Understanding Musculoskeletal Pain: Finding Relief and Taking Control
Written By Daniel Wray (Sports Physiotherapist & Mobility Coach)
That ache in your back, the stiffness in your neck, the twinge in your knee – these are common experiences we all face from time to time. Musculoskeletal pain, affecting our muscles, bones, ligaments, nerves, and tendons, can range from a mild annoyance to a significant disruption in our daily lives.
It's natural to feel concerned when pain strikes, especially if it's intense. However, it's reassuring to know that most musculoskeletal pain, even when it feels quite severe, is not a sign of serious underlying damage or pathology. Often, it can be related to things like muscle strains, sprains, overuse, or even just prolonged awkward postures. Our bodies are resilient, and these minor issues usually resolve with time and proper care.
When Should You Seek More Urgent Investigation?
While most musculoskeletal pain is not serious, there are certain situations where it's important to seek professional medical advice promptly. Be mindful of the following:
Lower Back Pain - Can Be Crippling but Is Rarely Serious Pathology
Severe pain that comes on suddenly and unexpectedly, especially after an injury.
Pain accompanied by other symptoms like fever, unexplained weight loss, or significant weakness.
Pain that radiates down your arm or leg with numbness or tingling.
Loss of bowel or bladder control.
Pain that is constant and progressively worsening, especially at night.
A history of cancer or other serious medical conditions.
If you experience any of these "red flag" symptoms, it's always best to err on the side of caution and consult a medical professional.
Simple Daily Habits and Strategies to Reduce Pain and Cope Better:
The good news is that there's a lot you can do in your daily life to manage and reduce musculoskeletal pain. Here are a few simple strategies to incorporate:
Some key areas to manage in improving Pain Control
Stay Active: Gentle exercise, like walking, swimming, or yoga, can help strengthen muscles, improve flexibility, and reduce stiffness. Find activities you enjoy and make them a regular part of your routine.
Practice Micro-breaks and Regular Movement: If you spend long periods sitting or in the same position, incorporate short, frequent breaks to move around, stretch, and change posture. Even a minute or two of gentle movement every 30 minutes can help relieve muscle and joint tension.
Be Mindful of Movement: Pay attention to your body when you move. Avoid sudden, jerky motions and lift heavy objects correctly.
Manage Stress: Stress can often exacerbate pain. Incorporate relaxation techniques like deep breathing, meditation, or spending time in nature.
Ensure Adequate Sleep: Quality sleep is crucial for muscle repair and overall well-being. Aim for 7-9 hours of restful sleep each night.
Consider Heat and Cold Therapy: Applying heat packs can help relax tight muscles, while ice packs can reduce inflammation. Experiment to see what works best for you.
Stay Hydrated: Drinking enough water is important for overall tissue health. This will range upwards from at least 2-3 litres per day depending on your circumstances
You Don't Have to Live with Pain – Help is Available:
Professional Physiotherapy guidance can help manage and improve your pain
Living with persistent musculoskeletal pain can be frustrating and limit your ability to enjoy life. Please remember that you don't have to accept pain as a normal part of your day.
At Physio Effect, our experienced team of physiotherapists is dedicated to helping you identify the underlying causes of your pain and develop a tailored treatment plan to address your specific needs. Our skilled practitioners are experts in assessing movement patterns, muscle imbalances, and joint mechanics. We utilize a variety of effective techniques, including manual therapy, targeted exercise prescription, and comprehensive education, all designed to help you reduce pain, improve your physical function, and prevent future problems.
Taking that first step to connect with the team at Physio Effect can make a significant difference in your quality of life. We're here to listen, understand your unique situation, and guide you on your journey towards a pain-free and more active future.
Summary
In conclusion, while musculoskeletal pain is a common experience, it doesn't have to dictate your life. By understanding the common causes, recognizing when to seek further advice, and incorporating simple daily strategies, you can take proactive steps to manage and reduce discomfort. Remember that expert help is available, and the experienced team at Physio Effect is ready to provide tailored support to help you regain comfort and get back to doing what you love.
thank you
Thanks for reading, please share with any friends, family or colleagues who could benefit.
We are always here to listen & help. Our specialist team can help you navigate and manage any ache, pain or injury.
You can Use the links to Book an appointment now or Contact us with any questions
Mobility - What? Why? When? How?!
Do you struggle with constant niggling joint and muscle pains? You workout regularly but still feel stiff all the time? Do you need help understanding and implementing better mobility habits and practices? If yes then this blog is for you! Modern stressful and busy lifestyles often mean we neglect flexibility and mobility practices. Long hours of static postures cause us to stiffen up & this compounds over weeks, months and years. It’s time to start organising your mobility practices to move better & feel better!
Improving mobility requires consistent structure, practice & effort!
Written By Daniel Wray (Sports Physiotherapist & Mobility Coach)
What is mobility?
Mobility is the ability to move freely and easily, encompassing physical movement, flexibility, balance, and environment access.
Mobility is vital for daily activities and exercise, impacting overall performance and quality of life.
Improving mobility enhances physical function, reduces injury risk, and fosters independence. Prioritising mobility supports long-term health and well-being.
5 barriers to mobility practice
Physical Limitations
Joint pain, muscle weakness, and neurological issues can hinder mobility exercises.Psychological Factors
Anxiety, depression, and lack of motivation can create fear of injury, impacting engagement.Access to Resources
Limited facilities, equipment, or expert access restrict effective mobility practice.Knowledge and Awareness
Lack of understanding about mobility's benefits inhibits participation.Environmental Barriers
Poorly designed spaces and clutter discourage movement, obstructing mobility practice.
stop sitting & start moving!
Sitting Is the New Smoking!
In our experience the main cause of reduced mobility and increased joint pain and stiffness is a sedentary job or lifestyle. Sitting for over 40 hours a week leads to negative consequences. What we see regularly in clinic is huge frustration from people in this situation who do actively find time for exercise, sport & gym classes.
“I go to the gym 4 times a week so why am I so stiff & sore?”
The problem with modern life stresses and lack of time mean many of us compartmentalise exercise to one point in the day for perhaps 1-2 hours. Out with that we are too static often sitting or standing at desks for long unbroken periods. Structured & planned exercise classes or sport is great but we must also find ways to inject short, varied, but regular amounts of movement into our everyday activities.
Tips to improve Mobility practice
Prioritise Side bends & Rotational Plane Movements
Incorporate Daily Stretching & Mobility Flows
Dedicate at least 10-15 minutes each day to stretching. Focus on major muscle groups and areas that typically feel tight, such as the hips, shoulders, and spine. Consistency is key to improving flexibility and joint mobility.Engage in Mobility-Focused Activities
Activities such as yoga, Pilates, and tai chi are excellent for enhancing mobility. These practices encourage controlled movements and can help increase your range of motion, balance, and overall physical awareness.Incorporate Micro Breaks
Aim to move for 2-3 minutes every hour as a minimum. Large simple movements of all major joints helps to create pressure changes and encourage healthy fluid balance in our tissues and joints reducing the cumulative build up of static postures.
Include Dynamic Warm-ups
Before engaging in physical activity, perform dynamic warm-up exercises. Movements like leg swings, arm circles, and torso twists can prepare your body for more strenuous activity and promote better mobility throughout your workout.Prioritise Functional Movements
A strong body is able to move in all planes of motion. A lot of gym exercises and routines can be too hinge like and robotic in nature failing to promote adequate movements in all planes. Incorporate good accessory training to include rotational, side bend and functional movements.
Example Mobility Flows For Daily Practice
Back Mobility Exercise Flow - Try this routine to gently mobilise your spine
Hip Mobility Flow - Try this exercise flow to mobilise and loosen up stiff hips
We love a 3 Point Bridge. Movement is medicine, start taking yours!
Summary
Improving mobility and reducing pain & stiffness is no simple task but it can be done! Take positive action and start today dedicating time for movement and stretching as often as you can. Spend some time analysing your current practice and training and see where you can improve.
We help people improve mobility & reduce pain and stiffness on a daily basis. If you need help to understand your needs and to design & implement a plan unique to your goals we can help!
thank you
Thanks for reading, please share with any friends, family or colleagues who could benefit.
We are always here to listen & help. Our specialist team can help you navigate and manage any ache, pain or injury.
You can Use the links to Book an appointment now or Contact us with any questions
Working From Home Survival Guide
Is working from home making you ill and injured? Are you in pain & stiffer than ever? Are you feeling isolated and unsupported? The risks are real and you are not alone. This survival guide will help you make better choices to reduce pain & stiffness and look after your body and mind. What are you waiting for? Follow our top tips to move more, organise yourself and have a positive impact on your physical and mental health
Is Working from home breaking you? Do you feel:
WFH health risks are very real
Stiff and sore?
back, neck, joint or muscle pains?
headaches or vision problems?
overwhelmed?
fatigued?
irritable?
low mood?
The risks of working from home (WFH) to physical and mental health are significant and real.
If you are feeling any of these issues you are not alone. You need to take positive action now and improve your individual situation.
Below we will list our top tips for how you can act now to prioritise your health. In Summary you need to :
MOVE MORE
GET ORGANISED
OPTIMISE YOUR WORKSPACE
Take Positive Action and Get Organised To Improve Your WFH Situation
top tip 1 - move more!
The single most important thing you can do to improve your WFH health is to move more. If you roll out of bed, grab a coffee then plant yourself at your desk with no movement or plans to move then you are brewing trouble. The NHS recommends reducing your sitting time significantly to improve your health and reduce the risks of type 2 diabetes, some cancers and even early death!
Are you already struggling with pain & stiffness in your neck, shoulders, back or hips? Check out these links to our previous blogs for advice, stretching and mobility instructional videos:
Movement Is The Key - Could you try Yoga?
When we are static (sitting or standing still) compressive and dehydrating forces are at work on our joints and soft tissues. All of our major body systems slow down and become sluggish which in the longer term contributes to significant health issues. The phase ‘Sitting Is the new smoking’ has been coined to highlight just how serious the impact of sedentary lifestyles can be
Movement creates positive pressure changes and improved fluid movement through our body as well as stimulating our body systems to be more active and alert. All of this helps to balance and reverse the negative effects of being static. Research shows us that movement and exercise can also help reduce stress and improve your mood.
Try these ideas:
Make time to move or you will get injured or sore
Rise earlier - Fit at least 10+ minutes of movement in before you hit the desk
Step challenge - Set a challenging daily step goal and go about smashing it. You need to prioritise time to walk. Try breaking it up into multiple smaller chunks (10-20 minutes x 2-3) throughout the day
Take breaks - Do not sit and rust at your desk! Take multiple complete breaks away from your desk and work. Walk, stretch or exercise, it doesn’t really matter, just take a break & move
Get outside - Combine fresh air & movement. Great for refreshing body & mind
Exercise for fun - Find something you enjoy and can commit to on at least a semi regular basis (2-3 x per week). Gym, walking, jogging, yoga, swimming etc.
Daily step targets are a great way to increase your activity. Get walking!
top tip 2 - organise yourself
Set Regular Break / Movement Alarms
Failure to plan is planning to fail! You need to actively organise yourself to make smarter, healthier choices and start reducing the negative impact of WFH.
We are great at making excuses for negative behaviour as it is generally the easier/lazier option. Get organised & remove barriers to promote positive action.
Try these ideas:
Plan Micro-Breaks - Aim to move away from your work for a minimum of 2-3 minutes every hour. Ideally combine this break with a little movement, stretching & breathing. 2-3 minutes of movement hourly is infinitely more important than trying to undo 8+ hours of static WFH with an end of day workout.
Set Movement Alarms - Use smart watches, desktop reminders or a simple timer to remind you when it’s time to get up and move. As already mentioned, ideally aim for a few minutes movement every hour as a minimum. Don’t ignore it! Get up and move.
Drink at least 2-3 litres of water every day
Create Dedicated Space - Dedicate some space at home away from your office or workstation setup to stretch, move & exercise. Get a yoga mat down, gather any small equipment like foam rollers or exercise bands and have it accessible. Removing the barrier of having to get setup each time you want to exercise will significantly increase your compliance
Measure Water Intake - Aim to drink at least 2 - 3 litres of water a day. Many people are chronically dehydrated and don’t even know it. This contributes massively to muscle and joint pain, headaches and general fatigue. Poor water intake increases your risk of dysfunctional metabolism and chronic diseases. Your tissues and body systems need water to function so give it to them! Use a water bottle to track your consumption and trigger better habits
top tip 3 - optimise your work space setup
When it comes to WFH there is no perfect workstation setup but you can improve and optimise in some areas. This article by the New York Times gives some further ideas on equipment and optimal desk setup. However, there is no point in forking out thousands on space age chairs and desks if you sit on you butt and barely move for 8+ hours a day.
You can’t buy your way to healthier WFH and you must still prioritise movement, regular breaks and a structure to your day that gives you balance physically and mentally. Once that’s in place see if you can implement some of the following ideas:
Stand Instead of Sit. Use a riser to optimise your screen and mouse position.
Stand Instead of Sit - Standing is probably the lesser of 2 evils and tends to naturally lead to a bit more movement and reduced pressure on some areas like the neck and lower back. If your work station allows it alternate sit to stand regularly throughout the day
Use Equipment & Aids - Optimise your sitting & standing postures by utilising equipment. Perhaps your employer can supply equipment such as a desk riser for raising the height of your monitor. Ergonomic chairs and variations of mouse and keyboards are available to promote better positioning and reduce repetitive strain. Access what you can & make arrangements that suit your own setup.
Stretch & Move - Our bodies love symmetry but unfortunately WFH and office based work in general promotes repetition with repeated postures, positions and static behaviours.
At risk of repeating ourselves here you need to counter static behaviours by moving your muscles and joints regularly through a large range and routinely in the opposite direction to the postures you adapt while working. For example to counter tightness in the hips and lower back from sitting we should target arching our lower back and lengthening our front hip and thigh muscles. Check out our Mobility blogs and Videos here.
‘Cobra’ Back Bend Stretch
Lunge Hip Opener Stretch
WFH can be happier and healthier
Summary
It’s time for you to take positive action if you want to improve your WFH situation. Stop making excuses, organise yourself and make healthier choices now to improve your physical and mental well being. It’s up to you!
thank you
Thanks for reading, please share with any friends, family or colleagues who could benefit.
We are always here to listen & help. Our specialist team can help you navigate and manage any ache, pain or injury.
Use the links below to Book an appointment now or Contact us with any questions
Pelvic Organ Prolapse
Pelvic Organ Prolapse - Signs, Symptoms and Treatment
PELVIC ORGAN PROLAPSE
WRITTEN BY JENNY DEVLIN, MSK PHYSIOTHERAPIST AND SPECIALIST WOMEN’S HEALTH PHYSIOTHERAPIST AT PHYSIO EFFECT. MCSP & HCPC
For a lot of people a diagnosis of, or even the thought of, pelvic organ prolapse is terrifying. It is extremely common though with the Royal College of Obstetricians & Gynaecologists suggesting that as many as 1 in 10 women over the age of 50 are affected. This number may well be higher with an increasing risk of complications after pregnancy and childbirth.
The good news is that many people are able to reduce or resolve their prolapse with the help of a pelvic floor physiotherapist. In this blog we explain more about Pelvic organ prolapse and look at how our experienced and specially trained Pelvic health Physiotherapists can help you.
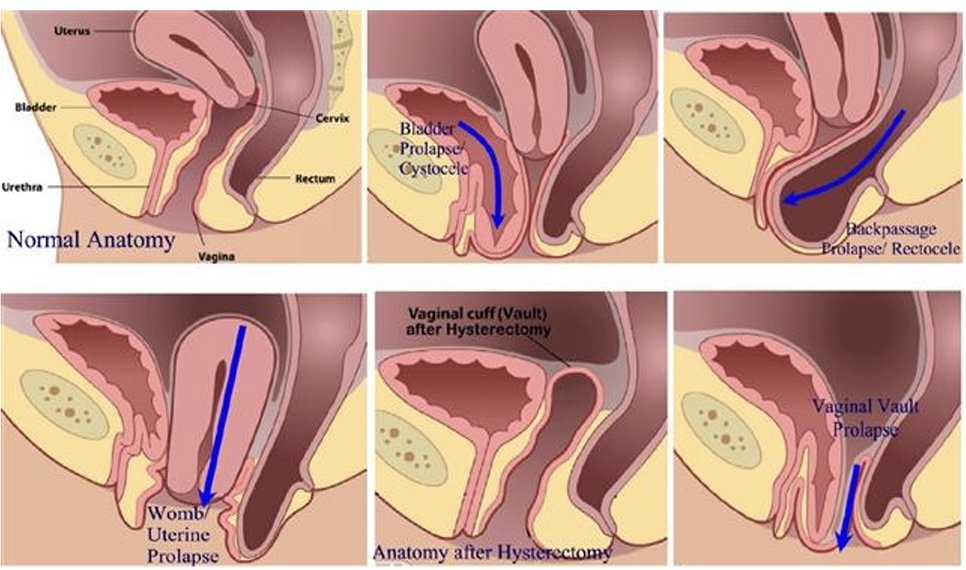
What is pelvic organ prolapse (POP)?
A pelvic organ prolapse occurs when a pelvic organ (or organs) bulge into the vaginal space. Strained, tight or weak muscles, ligaments or fascia can contribute to this. It can occur in different ways and we name the POP based on the organ that is not in its optimal position. A bladder prolapse (or cystocele) is where the bladder pushes against the front wall of the vagina. A uterine prolapse is where the uterus drops down into the middle of the vaginal space and a rectocele is when the rectum moves into the space at the back of the vaginal canal. You can also have a vaginal vault prolapse which occurs after a hysterectomy.
Pelvic Organ Prolapse
Symptoms of a pelvic organ prolapse
Prolapse affects everyone in a very unique way both physically and mentally. Some people live with prolapse and do not experience any symptoms. Other people can experience any number of symptoms which can be mild or affect your quality of life. Symptoms include:
pressure or heaviness in your pelvis area, which is often worse at the end of the day or with exercise
low back pain
urinary symptoms such as a slower stream, increased frequency or urgency to void, feeling of incomplete emptying of the bladder, urinary incontinence
bowel problems such as constipation, straining, feeling like the bowel doesn’t empty completely, increased frequency of bowel movements, faecal smearing (stool on the tissue after wiping clean), incontinence of faeces
Discomfort during sexual intercourse
Treatment options for pelvic organ prolapse
Pelvic Health Physiotherapy Assessment
Great news! Pelvic floor physiotherapy may be able to help with your symptoms of POP. Our team can help suggest changes you can make to your day to day routine to manage pressure on the organs, help with toilet positions to aid more effective urination/defecation.
Our specially trained Physiotherapists can assess muscle tension in the pelvic floor and abdominal muscles and help you to release this. We can also assess the strength and endurance of the muscles and teach you how to improve this if need be.
Physio instructed strengthening
We can guide you on correct strength and endurance exercises to help support the pelvic organs and the pelvis itself. This can help you in everyday functions when straining or lifting and on safely returning to sport. We can also make individual suggestions for more comfortable positions for intercourse.
Pessary For Pelvic Organ Prolapse
At Physio Effect our specialist team can assess and fit a pessary. A pessary is a device you wear inside the vagina, intermittently or continuously, to help hold things in position while you do the things you love. Once it is in place, you don’t feel anything but it can provide instant relief from that heaviness or pressure and can help with symptoms of incontinence too.
Cube Pessaries
Best of all once fitted these pessaries are designed for self management so you are in complete control and can remove and fit the pessary as required. After assessment and discussing your individual symptoms and needs our physiotherapists can help you decide if surgery might be the best route for you if conservative therapy has not worked.
We are here to help so please ask us anything. Hopefully this information makes things seem a bit less overwhelming and gives you hope that your symptoms can be improved. Give us a call or book in online for a full assessment and personalised treatment plan.
Sports Massage FAQs
Often, before, during and after a Sports Massage I get asked a handful of questions surrounding the topic. Therefore, I have compiled a list of FAQs that may help put a lot of minds to ease with this easy-to-follow guide and reason as to why you should get a Sports Massage.
Sports Massage – What is it and what does it do?
Warming up the rotator cuff
A Sports massage is a form of massage using a variety of simple and specialist techniques to manipulate the soft tissue of the musculoskeletal system.
1. Sports massage has been shown to increase muscle flexibility in the acute stage. This means that following your sports massage you will be capable of reaching positions that you struggled with prior to the massage. An example of this would be simply struggling to touch your toes, if this is due to extremely tight hamstrings then a sports massage on this area may improve blood flow to said area and allow you to reach the range you aim for.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7716682/
2. Sports massage has also been shown to aid recovery. As someone who trains you will undergo periods of stress on the body that will build up over time often known as DOMS (Delayed Onset Muscle Soreness). A sports massage will vastly improve circulation into these areas deprived of oxygen and nutrients and reduce the severity of the dreaded DOMS. https://bmjopensem.bmj.com/content/6/1/e000614
https://bjsm.bmj.com/content/32/3/212
3. Sports massage has also been proven time and time again to improve blood flow. In turn, this will enhance oxygen and nutrient delivery into your muscles which will allow them to feel better and more robust.
Who would benefit from a Sports Massage?
Everyone! From the everyday athlete and weekend warrior to the elite sports athlete. If you exercise as part of your routine then often, your body may begin to generate some fatigue, therefore, it is vital to take care of the impact your workouts are having on your body. (I am, however, quite the hypocrite as I do not receive massages as often as I should, whoops)
Muscle Energy Techniques (MET) on Hamstring
When can I train again after a massage?
As a general rule of thumb, I suggest that you should have a massage either on the same day as a rest day or the day before a rest day. The rationale for this, is that you will often feel tired after a massage as it puts your body into the ‘recovery process’. Post massage, your body activates the parasympathetic nervous system which allows your body to recover, thus, inflammation happens in the targeted muscle groups so that you can get back to a stronger condition afterwards.
Why do I get told to drink plenty of water after a massage?
After a massage, as previously mentioned, blood flow is improved, therefore the blood needs to continue to be oxygenated to deliver the right nutrients to the right areas, by drinking water this aids this process and prevents the risk of dehydration. As massage can be quite uncomfortable if your muscles are particularly tight, then your heart rate might spike during the treatment which will cause you to sweat and potentially cause fluid loss, so this by drinking enough you will replenish this lost fluid.
https://www.huffpost.com/entry/water-after-a-massage_n_2075604
How often should I get a massage?
There are various studies suggestive of different frequencies for massage but in my opinion, I believe it’s very individualised. A few examples are as follow.
If you are training at a moderate to high level (training 4-6 times a week), a sports massage once every 2-3 weeks should be enough.
During Jonny’s training, (one of our Physios here at Physio Effect) I had the privilege of providing him with a fortnightly sports massage which he found made a massive difference while pushing his body to new limits in his training to run the west highland way in December 2021. He stated that “the regular release of the muscle groups in my legs that were being overloaded with training allowed me to complete a 12-week plan for the first time ever without regular minor niggles to different muscles and joints in my legs. With the high training volume and a busy life, I often find it difficult to keep on top of my own soft tissue release and maintenance, so having the regular massage appointment in my diary meant I was able to focus my time and efforts into the more enjoyable training than torturing myself late in the evening on a foam roller. It also allowed me to have regular quality work done to a long-standing knee issue that I feel avoided it is flaring up beyond a manageable level in my training. I will absolutely be doing this on future training blocks for my various running events.”
If you are an elite athlete (2 a day sessions) then once a week would be the most optimal.
If you work a moderate to intense job/Occupational factors that involves either sitting in a compromised postural position or carrying heavy loads, then a massage once every 3-4 weeks would suffice. However, it is individual dependant as I myself, only get one every 2 months or so as it this fits my lifestyle.
https://www.onemassagetherapy.co.uk/how-often-should-you-get-a-massage/
Is a sports massage sore?
This is a question that is dependent on an individual’s pain tolerance, using myself as an example I get nervous prior to any form of body work as I expect it to be sore. However, using one of my managers Jonny as an example in which he won’t mind me saying, he is okay with a sports massage and tolerates them well, albeit that he receives them frequently and has built up a good tolerance towards them.
The pressure of the massage we provide is always adapted through the variety of techniques we use throughout the treatment so this will go from some light techniques in order to warm the tissue up at the beginning and end of the treatment with some specific deeper techniques throughout.
Gua Sha Scraping on the Pec (not the nicest)
When should I NOT get a massage?
If you have an acute injury (within the first 3 days of the injury occurring) I would not book in for a sports massage. The reason for this is that the injured area will be begin the healing process resulting in pain and inflammation. Massaging this area would only aggravate the injured tissue and potentially make the injury worse.
I hope this blog answers common queries and questions and we’ll be more than happy to answer any more questions either via email - reception@physioeffect.co.uk or by phoning us on 01412304766
Antenatal Pilates Classes at Physio Effect
Some exciting news! We have a NEW Antenatal Pilates class running in our studio within our Northside clinic at Borron Street. This physio-led Clinical Pilates class aims to prevent pregnancy related issues such as pelvic girdle pain (PGP), symphysis pubis dysfunction (SPD), posture related pain as well as a full body programme to prepare you for the birth of your child. During the class, you will be guided through an individualised programme relevant to your stage of pregnancy and any other issues discussed during your initial physiotherapy appointment.
WHEN: Wednesday evenings at 7PM from 21st October
**CLASS NOW FULLY BOOKED**
Please contact us below if you would like to be placed on our waiting list or if you wish to attend any of our other Clinical Pilates classes which will be a mixed group, but you will still be able to do an antenatal programme due to the bespoke nature of the class.
WHEN CAN I START?
As long as you have an uncomplicated pregnancy and your midwife/ doctor approves, you can begin from any time in your second trimester if you have no Pilates experience. If you have previous Pilates experience, you may begin earlier.
HOW DO I GET STARTED?
You will be required to have a 1:1 session with one of our physiotherapists before joining a class for the first time. During this appointment, your physiotherapist will be able to plan a bespoke Pilates programme for you based on your goals, requirements and stage of pregnancy. You will be introduced to the various Pilates props and equipment used during a class including the Pilates Reformer machine.
HOW MUCH DOES IT COST?
Antenatal Physiotherapy Appointment: £49
Single class rate: £25
6 classes: £120 (£20 per class)
12 classes: £220 (£18.3 per class)
You have flexibility to use the class blocks within the following time period:
● 10 weeks on a 6-class block
● 4 months on an 12-class block
WHAT HAPPENS IF I HAVE MY BABY BEFORE I USE UP ALL MY CLASSES?
You may use any remaining class credit towards our Crybaby Pilates Classes. This is our specialist Postnatal Pilates class which you may begin once you are at least 6 weeks postpartum after a non-complicated vaginal delivery or 8 weeks if you have had a C-section/assisted delivery with any complications.
CryBaby (Postnatal) Pilates Class
You are not your MRI: A Rehab Story.
Fiona Callan is a CrossFitter and Ultra-marathoner who injured her back in 2017. She had an MRI which showed an “L5/S1 disc bulge with nerve root irritation”. In this interview we discussed how she chose to avoid surgery and returned to the things she loved doing best.
Written by Mariam Kilpatrick, Physiotherapist and Clinical Pilates Lead at Physio Effect
Fiona Callan is a CrossFitter and Ultra-marathoner who injured her back in 2017. She had an MRI which showed an “L5/S1 disc bulge with nerve root irritation”. In this interview we discussed how she chose to avoid surgery and returned to the things she loved doing best.
Hi Fiona, thank you for taking the time to share your experience with us. Before we begin, tell us a bit about yourself…
I work in the NHS, primarily an office based job. Preceding my injury I was also studying for an MSc so basically spent all day and night sitting at a desk.
I started running in 2008, mainly 5k and 10k distance on roads but I wasn’t very good and didn’t enjoy it so moved to trail and hill running instead when I started gradually to increase my distance. I met some really cool people to run with as well. In 2012, I was talked into a trip to Nepal by a friend but it wasn’t until around 4 weeks to go that I found out he had signed me up to an ultra marathon. I didn’t even know what that was! It was sheer determination that got me through that and I really caught the ultra marathon bug.
In 2014 I started CrossFit as I thought some strength and conditioning type training would help with my running and I had no idea what I was doing in a conventional gym. The coaching and set workout approach has really worked for me and made me use muscles I didn’t know I had.
So the key question… how did you injure your back?
To be honest I’ve always had a bit of a lower back niggle, probably postural, but thought it would just go away. It was definitely something I started to feel more when I started CrossFit as I really had to use my back and core more than I had been doing running. Slowly I noticed it had started to affect my running, I had pain in my right buttock that shot down my leg now and again and my leg generally felt heavy. If I left it a few days it would go away but it meant I couldn’t really run or CrossFit as much as I wanted to.
It started affecting my job as I couldn’t sit comfortably for any period of time. I was travelling by train to Edinburgh at least twice a week which became difficult. On one journey I had to get off the train and go back to Glasgow as I couldn’t face sitting for an hour.
Then during a workout involving a barbell I cried so much I had to admit that something wasn’t right.
My initial symptoms were primarily in my lower back, there was a build up of pressure around my stomach and back even when I bent over the sink to wash my face. I tried to keep active but really scaled back on what I was doing. I kept up my hill walking as this is an activity I love doing with my nephew – I used poles and made Ewan carry my bag as he’s the young one! I tried running but could only manage 1k before I felt my back stiffen.
One Saturday I went walking with Dad and Ewan in the Lake District. It was an amazing day. The hill wasn’t too hard; we took our time and enjoyed it. It was the shooting pain in my right leg that woke me up early on the Sunday morning. I tried to stand up but my leg just wouldn’t work. I limped to the bathroom hanging onto the wall and at that point I knew there was something seriously wrong. It sounds dramatic but I genuinely felt paralysed down that whole side of my lower body, first thoughts were ‘I’ll never run again!’ and panicked. My boyfriend called NHS24 and a nurse managed to calm me down and suggested I took paracetamol with ibuprofen and try find a comfortable position until a doctor could get to me. A few hours and one injection later the pain had dulled. He said it was my sciatic nerve; I should try to relax and spend less time sitting down!
What treatment did you seek initially?
I got an appointment with Jonny who did some needling on my lower back/ glutes and gave me some exercises to do. I am the most impatient person and after a week of exercises I didn’t feel any different so I saw another physio (sorry!) who basically told me the same thing and gave me the same exercises. I really was in denial about how serious it was. I spoke to coaches in the gym, chatted to other runners and did a lot of Googling but all the answers were the same.
It was the mental part I actually found the toughest to deal with. I have made so many friends through running and CrossFit and my social media is full of it too so I was always seeing and hearing about all these amazing runs and PBs. I just felt stuck and disconnected. I saw my GP as I really felt like I was struggling to cope. People were always asking how I am and telling me I should ‘do this and do that’ and eventually I just got fed up talking about it. My GP didn’t really help me; she referred me to her physio friend but I didn’t go.
At the same time, Jonny had referred me to see Mariam for Clinical Pilates and it was during my consultation that she suggested some short term medication for my nerve problem in my right leg. I went to another GP for this and as well as giving me the medication, he was really keen to get me back running and to the gym so he referred me for an MRI.
What happened after your MRI?
I was really lucky in that I got an MRI pretty quickly. A few weeks after the scan. I received a letter with a hospital appointment but with no other information. Frustrating and worrying. I thought well there must be something not quite right and because of my problem with patience, I called the GP and asked him to give me a brief overview of the scan. He said he could see a disc bulge and I should continue doing my physio exercises until my appointment (with the consultant). I had just started with the Clinical Pilates class so I let Mariam know the issue and she tailored exercises for me until I found out more about the problem.
How did you feel after speaking to the neurosurgeon?
I remember getting a phone call from a surgeon in the spinal unit and it made me feel sick. I actually don’t remember what he said to me as the idea of back surgery just terrified me. I wasn’t exactly in crippling pain so the idea of surgery just felt a bit extreme to me. This was something I definitely wanted to avoid. I just really trusted my physios and they really believed I could get better without it. I didn’t feel that my pain was bad enough for surgery – for me this was the last resort.
At the appointment, the doctor went through my scan which I found fascinating. I actually felt a bit of weight come off my shoulders when I could physically see the issue. It had been hard to accept when I didn’t know for sure what the problem was but there it was clear in front of me. She then told me that they would do surgical intervention if I was getting sharp pains down the top of my leg. I told her I had that a few weeks before but it had been getting much better. We left it at that and I was told to get in touch if anything changed.
I had so many conversations with my boyfriend, my parents (and myself) and decided that it wasn’t the end of the world if I couldn’t run 50 miles or couldn’t deadlift 100kg as long as I could stay active. I would just scale back what I was doing.
You've spent the best part of a year doing some serious rehab with Clinical Pilates. In your own words, what is it and how did it help you?
I had done a bit of Pilates before as I’d read and heard it was good for runners. It was one of those things I struggled to stick to because I never left the class feeling like I’d worked hard and my issue with patience didn’t help. When I told my boyfriend about it he signed me up for 6 weeks because he knew I’d have to go if he paid for it! I noticed a huge difference after these 6 weeks.
It is basically pilates but physio-led so your exercises are all tailored to whatever issue you may have so we’re all doing something different generally. It’s a small class but everyone is in the same boat and really friendly. Mariam checks in with you regularly during the class and pushes you when you’re ready but also changing exercises if something isn’t quite feeling good.
I expected my exercises to all be lower back focused as that’s where my injury was but actually they’ve been full body movements. As well as having a stronger back, I feel stronger and much improved posture. Mariam also spent some time working on my legs, particularly my right leg as the nerve had been affected and I had limited movement and very little strength.
Eventually you returned to CrossFit and trail-running. How long did that take from when you first injured yourself?
I was always doing a scaled back version of CrossFit and a bit of trail running while I was injured but I was mindful of undoing my hard work. It was important to me mentally that I kept in touch with coaches/ friends in the gym and my runner friends.
I accepted my injury in May 2017 and started Clinical Pilates in the October. In May 2018 I was a more confident runner so decided to train for a race following a plan, building up in distance and I finished the Mad Hatters Half Marathon and the Glentress Half Marathon with a PB and no back or leg pain. Not quite back at ultra marathon distance but I’m actually enjoying the shorter runs at the moment. In June 2018 I started back at CrossFit and noticed that I’m better at a lot of the movements as I actually use my back and core as I should. I’m always conscious of loading too much weight on bars and I know certain movements still aggravate my back but I know when to stop and I just need to gradually build my strength back up. I was asked if I’d like to be part of a team from the gym for a CrossFit competition, I said yes why not I can try and we finished in 3rd place with no back pain!
Most people seek the "quick-fix" or miracle cure. What advice would you give them?
Your back is such a major part of your body so decisions on surgery should never be made lightly. Unless a professional is telling you there is no other option, I would encourage people to commit to the exercises and rehab, spend less time being sedentary and stay active by doing anything you find fun.
Working through this injury has taught me so much about my body and my lifestyle as well as making me a better runner and CrossFitter. This is all coming from the most impatient person!
SEEKING GUIDANCE? WE CAN HELP
Our experienced team at Physio Effect Glasgow are specialists in back pain and have helped 1000s of people recover and get back their quality of life. We talk the talk and walk the walk and will combine exercise based rehab such as Clinical Pilates with highly skilled hands on therapies to ensure you get the best possible treatment.
Most importantly we will listen and work with you in partnership to identify your specific issues and formulate an agreed unique treatment plan. We will relieve your back pain and give you long term self management strategies to strengthen your back and reduce the chance of pain relapse.
Please contact us if you have questions about our physiotherapy and Clinical Pilates services. Book an appointment and get your journey to back pain recovery under way.
Back Pain - A Self Help Guide
Back pain is very common. It’s frustrating at best and debilitating at worst. This guide will help you develop strategies for long term change to get rid of back pain and stay pain free long term. No magic bullet or ‘Guru’ advice here, just sensible and actionable tips allowing you to take control and start your journey to a pain free back.
Written by Daniel Wray (BSc Hons Physio/ PG Dip Sports Physio)
Back Pain?
We’ve all been there…..
Why does my back hurt?
Back pain is common, if you’re reading this i’m sure you have suffered at least one episode of back pain in your lifetime and in all likelihood more than that. It’s frustrating and restricting and can have a huge negative impact on your quality of life.
There are many reasons for back pain and unfortunately it’s rarely a quick fix. The most common form of back pain is often referred to as mechanical pain which is an umbrella term describing dysfunction in the soft tissues and joints preventing or impeding normal function. This may be stiffness, weakness, muscle shortening, joint wear and tear or any combination of these plus other factors.
In the absence of acute trauma back pain rarely appears suddenly or overnight and for most it’s a gradual and cumulative process related to lifestyle. Our modern lifestyles are simply too sedentary with too many hours spent in static positions meaning our joints and muscles don’t get the movement stimulus they need to stay flexible, hydrated and healthy.
For many people what began as a minor back ache or stiffness spirals steadily into chronic pain and disability and it can seem like you’re stuck in a repetitive cycle of injury and pain. We try to make changes but the daily grind means we continue to rack up hours of sedentary, static, and repetitive behavior trapping us in this negative cycle. The pain can force further lifestyle changes meaning less movement and exercise which reinforces the negative cycle and it can seem impossible to break free. Having a dodgy sore back slowly becomes the norm and we just accept it and carry on.
It’s not all bad news - here’s what you can do…
It all seems pretty grim and depressing right? Well the good news is that for the most part the majority of back pain, even when extremely painful and debilitating, is not due to serious pathology and it can get better. There are of course exceptions to this and we would always advise you seek advice from a qualified health professional if you have serious concerns about your back pain.
The bad news, if you look at it that way, is that the fix is rarely instant and usually requires significant effort on your part to make lifestyle changes and prioritise time every single day to look after your back. Of course if you Google hard enough (we’ve all done it) you will find some ‘Guru’ promising an overnight fix in exchange for a significant amount of your hard earned cash but truthfully the magic bullet doesn’t exist. Below we have listed some strategies you can implement to make a real difference.
6 self help strategies to help manage back pain:
1- Keep moving. Complete rest is not going to help and generally increases stiffness, pain and fear avoidance behaviors. Of course we must adapt our movement depending on the level of pain and there may be a need to avoid certain postures, positions or movements for a short period of time which is fine. I don’t recall any scenario with a patient where we couldn’t find at least one simple movement they could do to keep some gentle activity in their back to promote healing and relaxation while building confidence that they are not going to stuck in pain forever. Experiment with different movements and stretches (see below video) gently and slowly and see what you can manage comfortably and that will give you a starting point which you can gradually add other movements to as your pain allows.
Lunge with arm and spine rotation
2- Establish routine & be proactive not reactive. You need to act consistently and with purpose. Don’t wait until your pain is crippling to decide you need to try some exercises to relieve it. Even if you’re feeling okay find a rhythm that allows structured gentle movement and exercise to be part of your daily routine ideally multiple times a day. Frequent exercise micro breaks to interrupt static postures will reduce the build up of pressure and stiffness and are more desirable than trying to undo hours of sedentary behaviour with a single bout of exercise. Think 2-3 minutes activity every hour rather than a 30 minute blast at the end of the day. Use a timer to remind you.
3- Accept responsibility & seek guidance. It is your body and your back and you need to find a way forward, nobody can do it for you. Don’t pass responsibility onto any therapist (no matter what some ‘Guru’ promises) and assume that by chucking money at it that will be enough to fix you. Do find help from someone you trust who has your best interests at heart and involves you in all aspects of any treatment or rehab plan. Passive treatments such as massage, acupuncture, and manipulation can be great for pain relief but long term are only as good as the agreed exercise plan and responsibility you take in changing your lifestyle. Be wary of any therapist promising to fix you but providing no education or prescription of exercises you can use to help yourself.
4- Exercise for fun. Find a form of exercise you genuinely enjoy and commit regularly to it. Don’t drag yourself to the gym if you hate every minute of it, exercise should be enjoyable and a way to relax your mind as well as your body. Try new things and see what you enjoy. Ultimately your long term compliance will wain if you pursue something because you feel you have to rather than because you really want to.
Back Strengthening - Extensions on the GHD machine
5- Manage stress. One of the biggest silent assassins to any life goal is high stress levels. You can have all the good intent in the world in changing lifestyle and exercising more but if you are under high levels of stress you can easily sabotage any progress. I realise this is a broad blanket statement and stress management is a big topic beyond the scope of this article but at the very least be aware of how it contributes and can damage your progress, then start to look for solutions.
6- Be patient. You won’t change things overnight and chances are you will have many peaks and troughs in your recovery. This is normal. Try to be patient and remember a backward step with increasing pain symptoms is not the end of the world, try to continually adapt but keep taking positive actions even when you feel frustrated and annoyed. If you follow the steps above you should see over time the more severe episodes of back pain decrease while your ability to manage and recover from any acute episodes will improve.
Picking Exercises - Where to start?
It’s imperative to get moving ASAP with pretty much every kind of back pain or injury but the exact type of exercise or stretch you choose to get started with will differ depending on your level of pain, stiffness and disability. Below is a back mobility exercise flow covering a multitude of different exercises and positions. Try it but STOP if you feel any specific movement aggravates your pain. At most a slight awareness of stiffness or aching is permissible but do not force anything and take it slowly and gently.
You may decide that only a couple of these exercises work for you in your current situation and that is fine, identify what you can do and exclude what you can’t. That will be your start point and I would advise doing these exercises a minimum of 3 times per day but ideally more frequently at least initially. As you become more comfortable hopefully you can add more of the movements to your repertoire.
Long term most people will require a combination of strength and flexibility exercises but it is important that these are specific to your own individual requirements. The routine below is provided as a starting point but is not all encompassing so please seek advice on your own needs but do use these stretches to try and initiate positive change through movement. The exercises are broken down individually in the pictures below the video & you can download a PDF cheatsheet to keep for your reference at the end of this blog.
Back Mobility Flow Video:
Seeking Guidance? We Can Help
Our experienced team at Physio Effect Glasgow are specialists in back pain and have helped 1000s of people recover and get back their quality of life. We talk the talk and walk the walk and will combine exercise based rehab with highly skilled hands on therapies to ensure you get the best possible treatment.
Most importantly we will listen and work with you in partnership to identify your specific issues and formulate an agreed unique treatment plan. We will relieve your back pain and give you long term self management strategies to strengthen your back and reduce the chance of pain relapse.
Please contact us if you have questions or to book an appointment and get your journey to back pain recovery under way.
Exercise Breakdown:
Here is a breakdown of each of the exercises included in the back mobility flow video. These are available in a handy PDF download from the Subscription box at bottom of the page.
Exercise 1
Cat & Camel Stretch
Begin in all 4s position. Cat posture - Allow your spine to soften and hollow along its entire length. Tilt your tailbone gently to the ceiling. Relax you lower back, rib cage, shoulders and neck
Camel Posture - Arch your whole spine slowly and gently to the ceiling in one large ‘C’ shape. Tuck your tailbone between your legs
Hold each position for around 10 seconds. Transition from one to the other 6-8 times.
1- Cat Pose
2- Camel Pose
Exercise 2
Childs Pose to Cobra
Begin in all 4s position. Childs pose - Gently sit bottom back towards heels as far as is comfortable opening knees and hips softly and as required
Cobra Pose - Allow weight to come forward and lower hips gently to floor. Stay relaxed in hips and lower back and if required bend elbows slightly so that hips can rest in contact with floor.
Hold each position for around 10 seconds. Transition from one to the other 6-8 times
1- Childs Pose
2- Cobra Pose
Exercise 3
Childs Pose Side Bend
Begin in Childs Pose - Walk you hands around to one side into side bend aiming for at least a 45 degree angle, you should feel a good stretch down your side. Hold 20-30 seconds.
Walk hands around in same way to other side and again hold 20-30 seconds in side bend.
Repeat 2-3 times on each side
1- Childs Pose
2- Side Bend Right
3- Side Bend Left
Exercise 4
Lunge Hip Flexor Opener
Begin in Lunge position. Gently engage your lower tummy muscles and tuck your pelvis in. Aim to feel a stretch in the front of your hip and top of thigh
Gently engage your buttock muscles and lean slightly forward taking care not to arch your lower back
Hold the position 30-60 seconds. Repeat 1-2 times left and right
1- Lunge Hip Flexor Opener
2- Lunge Hip Flexor Opener - Forward Lean
Exercise 5 - Part 1
Lunge Hip Opener with Alternate Arm Rotations
From Lunge position reach hands forward and rest on floor beside front foot. Take outside arm and reach under and between legs ‘threading the needle’ holding for a few seconds
With the same arm rotate outward and upward toward ceiling trying to get arm to a straight vertical position, hold for a few seconds then return to ‘thread the needle’
Repeat this 10 times
1- Lunge Position Hands Forward on Floor
2- Lunge Position Hands Forward ‘Thread The Needle’
3- Lunge Position Hands Forward - Rotate arm vertically reaching for ceiling
Exercise 5 - Part 2
Lunge Hip Opener with Alternate Arm Rotations
After completing Part 1 of this series stay in the same position but extend out your back leg as far as is comfortable
Take inside arm now and rotate upward to the ceiling trying to achieve the straight arm vertical position, Hold for a few seconds
Bring the same arm down and with bent elbow drive your elbow towards the floor down the inside of your shin. Hold for a few seconds then rotate back to the vertical arm position
Repeat this 10 times
4- Lunge Position Extend Back Leg
5- Lunge Position Inside Arm Rotate to Ceiling
6- Lunge Position Inside Elbow Drive to Floor
Exercise 6
A-Frame Walk to Squat
From the all 4s position drive your hips into the air with straight knees and gentle lower your heels towards the floor into the A-Frame (it does not matter if you can’t fully extend knees or reach the floor with your heels). Hold for 10 seconds feeling stretch in back of legs
Keeping hands on floor slowly walk feet in towards hands and slowly sit down into a squat, hold for 10 seconds
Walk back to A-Frame position and hold for another 10 seconds
Repeat 4-6 times
1- A-Frame Position
2- A-Frame Walk to Squat
3- A-Frame Walk to Squat 2
4- Finish in Squat
Thank You
Thank you for taking the time to read this post, we sincerely hope that you find it useful and can use it to implement some positive changes and reduce your back pain. Take your time and work at your own level but be persistent and try to gradually improve on your own baseline.
Please download your own FREE PDF Cheatsheet to keep and to help with your practice and share this post with anyone who could benefit. If you have any questions or comments please just ask we would love to hear from you. Stay healthy and move well.
Restore your core after pregnancy: A safe return to exercise
Returning to exercise after having a baby can be daunting & difficult. It is possible to cause yourself more harm than good if you return too soon or to the wrong type of exercise. This blog looks at the evidence and guidelines for returning safely to post-natal exercise and the specific benefits of Post-natal Pilates in restoring your Pelvic Floor muscle function, reducing Diastasis Recti and rebuilding your core strength and function. A FREE 30 minute Post-natal Pilates class is linked for you to try.
Written by Mariam Kilpatrick - Physio, Clinical Pilates Instructor, Ultra-marathon runner & Awesome mum
After 9 long months, finally, your cute little bundle of joy has arrived! Goodbye to feeling like a bloated whale and goodbye heartburn. Say hello to sleeping on your tummy and to eating stinky cheese & sushi again. You’re keen to get back to exercise, get that endorphin rush and reclaim your pre-pregnancy body! You’ve had your 6 week check-up and your doctor has given you the all clear to exercise. Yay! BUT…yes there is a but. You can sometimes do more harm than good if you push your body beyond what it is ready for. Here we review the guidelines for returning safely to postnatal exercise and look at the specific benefits of Postnatal Pilates which include improved Pelvic Floor function and reduced Diastasis Recti (abdominal separation). Read on for more….
As the saying goes, you shouldn’t build a house on a weak foundation.
For many women, it has become a common thing to accept “a little bit of wee escaping” with a sneeze or running for the bus, just because you’ve had a baby. But no matter what age your baby is, either 6 weeks or 6 years, this should not be the perceived norm. Some women may feel embarrassed to raise their concerns around continence and other intimate issues but this should never be the case. Please seek professional advice early, as with the right help and guidance, these issues can and should be addressed.
The Pelvic Floor Muscles
Your Pelvic Floor is a hugely important part of your body. It is made up of layers of muscle and connective tissue. These layers stretch like a hammock from the tailbone at the back, to the pubic bone in the front. They support your pelvic organs and control your bladder and bowel movements. The front passage (pee hole), the vagina and the back passage (poo hole) all pass through the pelvic floor muscles. Throughout your pregnancy, your pelvic floor has carried the weight of your baby, the placenta and a 50% increase in blood volume! As such, this will greatly affect its ability to do its job properly compared to pre-pregnancy function. It is therefore vital to work on these muscles after having a baby, regardless of the type of birth you had (whether vaginal or C-section).
Let’s practice how to correctly engage your pelvic floor…
Take a deep breath in, fill your lungs completely and allow your pelvic floor to relax.
As you breathe OUT, close your back passage as if you were holding in a fart, then pull upwards and inwards towards your front passage to close it, as if you were holding in a pee.
Visualise trying to "squish" your anus (poo hole) to your urethra (pee hole) towards your pubic bone.
Do this without clenching your butt cheeks, your jaw or tensing your neck and shoulders (tricky, huh?)
Let everything relax again as you breathe in.
Repeat x 10Now try and engage your pelvic floor as above in 10 x quick flicks on and off.
*Practice turning your pelvic floor on in both sitting and standing positions
**Practice turning your pelvic floor on when doing things at the same time like picking your baby up from his/her cot or picking a toy up from the floor.
Why do I still look pregnant months after giving birth?
In the latter stages of pregnancy, the connective tissue or fascia between your outermost abdominal wall (your six-pack muscles) can thin out/stretch to allow for a growing baby bump. After giving birth, you can be left with a gap between the two sides and sometimes it can look like you are still pregnant i.e. the dreaded “mum-tum”. This is called a Diastasis Recti or abdominal separation, a common condition that causes a lot of grief for many mums. However, like any muscle in the body, these can be addressed and worked on with specific corrective exercises - all hope is not lost! The key is to target the deep layer of abdominal muscles. This may mean avoiding certain traditional core stability exercises initially (e.g. sit ups and planks). Your deep abdominal muscles have functional connections to - guess what - the pelvic floor…so it’s a win-win situation all round!
Postnatal Pilates
Pilates is a great form of exercise to target the working relationships of your pelvic floor and core muscles (abdominals and diaphragm) especially in the first few months after having your baby. The benefits of Pilates include:
Strengthening your Pelvic Floor
Targeting your deep abdominal muscles to help heal Diastasis Recti
Addressing muscle imbalances that may be contributing to lower back pain or pelvic girdle pain
Targeting postural muscles of the back, neck and shoulder girdle
Postnatal Pilates Class at Physio Effect
Here is a short taster video of a postnatal Pilates workout:
We Want To Help You Get Your Body Back On Track
Physio Effect specialises in helping mums recover their health, fitness and confidence after having a baby. Our Cry-Baby Pilates classes where new mums attend with their babies has been a great success and very popular. We are working hard to bring this content to full digital online form so that all mums everywhere can enjoy and benefit from this safe, structured and fun specialist postnatal program. For advanced notice of when this course is available and for special early-bird promotional rates please register for your free sample class below and we will keep you informed.
Want to read some REVIEWS about our classes from other mums? Click the links & read below: Yell.Com Reviews or Facebook Reviews
The cry baby Pilates classes led by Mariam were an absolute highlight of my maternity leave. They offered important rehab for all the changes to my body left by pregnancy and a c-section and the strengthening work got me back safely running sooner than I expected - yay! The classes were warm, friendly and supportive and my baby Helena loved meeting the other babies too (as well as getting cheeky cuddles from Mariam). Couldn’t recommend more highly to new mums!
Katherine C via Facebook reviews
I’ve recently completed 2 blocks of Crybaby Pilates with Mariam & would highly recommend it for postnatal recovery. Mariam was great at making you feel relaxed, gradually building up the intensity of the exercises over the weeks so it wasn’t too daunting in the beginning. I liked how the exercises also allowed you to interact with your baby. The classes are small enough that you get the opportunity to get to know the other mums & babies, which helps you feel completely at ease in the class too. I now feel back to my pre-baby self & body, ready to start running & hitting the gym! Thank you!
Keri. L.K via Facebook reviews
Would you like a FREE 30 minute Specialist Postnatal Pilates class to try?
Please Click the following link to register & we will send you a video link to enjoy
Returning to Exercise - What do the guidelines say?
In the first six weeks after giving birth and when you feel you are able, you may commence your pelvic floor and abdominal exercises, functional bodyweight movements, as well as low impact cardiovascular exercise such as walking.
From six weeks onwards (or a little longer if you’ve had a C-section), you may commence light resistance exercise such as Pilates and light weights training.
The earliest you should start high impact exercise such as Running/HIIT/Bootcamp is between 3-6 months after having your baby. This of course may differ from person to person depending on the type of birth you had. A recent study for guidance in returning to running post pregnancy by some expert pelvic health physiotherapists can be found here
Seek Help & Advice Sooner Rather Than Later
As with everything in life, there isn’t a one size fits all when it comes to returning to exercise after pregnancy. Factors that need to be considered include:
Type of birth you had; was it a straightforward vaginal birth, a vaginal birth with complications such as forceps delivery/episiotomy/tears, a C-section? The timescales may be different for each case!
Previous level of exercise (e.g. were you a runner/gym-bunny/Crossfitter before pregnancy?)
Experiencing symptoms of lower back pain, pelvic or pubic pain, leakage and/or feeling of vaginal heaviness (which could be a sign of pelvic organ prolapse), coccyx/tailbone pain (which could be a sign of a hypertonic or tight pelvic floor)
Are you currently breast-feeding? Pregnancy hormones stay in the body for about three months postpartum, continuing to loosen joints, muscles, tendons and ligaments as they did in preparation for delivery. For those breast-feeding, hormones can still have a loosening effect even months after you stop.
If you are unsure, it is advisable to seek help from a specialist trained physiotherapist or a pelvic health practitioner.
If you would like to chat to one of our physiotherapists you can use the link below to book an appointment. Or if you prefer send us a message with any questions you have and we will get back to you as soon as we can.
Thank You
Thanks for taking the time to read this guide, we hope you find it useful. Please share with anyone else who might benefit and if you have any questions comment and let us know. Please subscribe for regular updates and advice on everything health and fitness related - Zero spam promise.
Postnatal Pilates at Physio Effect
Stiff back? Try our simple six step mobility routine
6 step mobility stretch routine to ease back stiffness and relieve back pain. Practice daily and you will see improvements in your range of movement and alleviate tension, stiffness and pain in your back.
Back Pain?
We’ve all been there…..
What’s up with my back?
We’ve probably all struggled with a stiff achy back at some point. The reality is that our modern lifestyles are often dictated by technology and we just don’t move enough to maintain healthy joints and soft tissues. If you truthfully counted up how many hours per day or week you spend in sedentary / static positions whether working from a computer, driving, or binge watching TV and social media what would that number look like? How would it compare with hours spent being active, stretching, moving and getting some exercise? Chances are you are in the majority with your results skewed in the wrong direction and sedentary hours winning hands down.
Even for those of us who do exercise regularly it’s often at the back of a long day of not moving much. There is often a misconception that working out a few times a week should be adequate to ward off the stiffness and tightness that comes from our daily work routines. While of course some exercise is better than none what most of us need to do is work harder at incorporating small amounts of varied regular movement into our everyday routines. Micro breaks of several minutes every hour are a great way to break up the day & if you can practice a few hip and back movements and stretches with these then that’s a winning combination.
Most of the back pain we suffer is not serious (but do ensure you have checked with a medical professional) even when the pain and stiffness reach fairly extreme and debilitating levels. It is most often a cumulative and gradual process which results in reduced joint and tissue flexibility and a lower threshold or tolerance for simple tasks.
You may have a sensation of achy stiffness and tightness in your back and feel the need to fidget and change position constantly just to get comfortable. Sometimes acute painful events occur as the result of a simple daily task like putting on your socks and you can feel trapped in a cycle of stiffness, pain and vulnerability.
These symptoms most often aren’t indicative of something seriously wrong but rather your body is sensing changes it doesn’t like and is giving warning that something needs to change. X-rays and MRI scans aren’t normally helpful, unless being used by a medical professional to exclude other suspected pathology, and more often than not can cause confusion and fear which can negatively impact behaviour and recovery.
What can I do?
All is not lost and it’s never too late to make positive change. For most of us that can be very simple in the form of developing strategies that encourage us to move more in our daily routines. Try these pointers:
Be positive and take action of some kind. Note anything that seems to help or has a positive effect on how you feel and work to develop that
Focus on what is within your control to change and don’t worry or get hung up on the things you cannot do or cannot change
Develop simple daily habits and routines that encourage an increase in regular movement, exercise, and stretching
If you plan on being static/sedentary for extended periods plan micro-breaks of 2-3 minutes at least every 60 minutes and include some walking and simple stretching movements
Try to find a physical activity or exercise that you enjoy and doesn’t feel like a chore as you are much more likely to perform it regularly and achieve a long term change
Consider other lifestyle factors where you can implement simple change - e.g. drink more water, increase sleep, meditate or practice deep breathing & reduce daily screen time usage.
Let’s get started!
Below is a mobility routine for your back of 6 different exercises performed as a movement flow to get you started. Always begin slowly and gently and work within your own comfort limits. If you can only do part of the movement or a modified / reduced range that is fine, just do what you can. Try them every day and perhaps even multiple times per day if you’re able and you will gradually start to feel better and move better. Ideally try the whole routine or you can divide it up into single exercises and see which ones you find give you the most relief but aim to practice all the movements every day.
Back Mobility Flow Video:
Exercise 1
Cat & Camel Stretch
Begin in all 4s position. Cat posture - Allow your spine to soften and hollow along its entire length. Tilt your tailbone gently to the ceiling. Relax you lower back, rib cage, shoulders and neck
Camel Posture - Arch your whole spine slowly and gently to the ceiling in one large ‘C’ shape. Tuck your tailbone between your legs
Hold each position for around 10 seconds. Transition from one to the other 6-8 times.
1- Cat Pose
2- Camel Pose
Exercise 2
Childs Pose to Cobra
Begin in all 4s position. Childs pose - Gently sit bottom back towards heels as far as is comfortable opening knees and hips softly and as required
Cobra Pose - Allow weight to come forward and lower hips gently to floor. Stay relaxed in hips and lower back and if required bend elbows slightly so that hips can rest in contact with floor.
Hold each position for around 10 seconds. Transition from one to the other 6-8 times
1- Childs Pose
2- Cobra Pose
Exercise 3
Childs Pose Side Bend
Begin in Childs Pose - Walk you hands around to one side into side bend aiming for at least a 45 degree angle, you should feel a good stretch down your side. Hold 20-30 seconds.
Walk hands around in same way to other side and again hold 20-30 seconds in side bend.
Repeat 2-3 times on each side
1- Childs Pose
2- Side Bend Right
3- Side Bend Left
Exercise 4
Lunge Hip Flexor Opener
Begin in Lunge position. Gently engage your lower tummy muscles and tuck your pelvis in. Aim to feel a stretch in the front of your hip and top of thigh
Gently engage your buttock muscles and lean slightly forward taking care not to arch your lower back
Hold the position 30-60 seconds. Repeat 1-2 times left and right
1- Lunge Hip Flexor Opener
2- Lunge Hip Flexor Opener - Forward Lean
Exercise 5 - Part 1
Lunge Hip Opener with Alternate Arm Rotations
From Lunge position reach hands forward and rest on floor beside front foot. Take outside arm and reach under and between legs ‘threading the needle’ holding for a few seconds
With the same arm rotate outward and upward toward ceiling trying to get arm to a straight vertical position, hold for a few seconds then return to ‘thread the needle’
Repeat this 10 times
1- Lunge Position Hands Forward on Floor
2- Lunge Position Hands Forward ‘Thread The Needle’
3- Lunge Position Hands Forward - Rotate arm vertically reaching for ceiling
Exercise 5 - Part 2
Lunge Hip Opener with Alternate Arm Rotations
After completing Part 1 of this series stay in the same position but extend out your back leg as far as is comfortable
Take inside arm now and rotate upward to the ceiling trying to achieve the straight arm vertical position, Hold for a few seconds
Bring the same arm down and with bent elbow drive your elbow towards the floor down the inside of your shin. Hold for a few seconds then rotate back to the vertical arm position
Repeat this 10 times
4- Lunge Position Extend Back Leg
5- Lunge Position Inside Arm Rotate to Ceiling
6- Lunge Position Inside Elbow Drive to Floor
Exercise 6
A-Frame Walk to Squat
From the all 4s position drive your hips into the air with straight knees and gentle lower your heels towards the floor into the A-Frame (it does not matter if you can’t fully extend knees or reach the floor with your heels). Hold for 10 seconds feeling stretch in back of legs
Keeping hands on floor slowly walk feet in towards hands and slowly sit down into a squat, hold for 10 seconds
Walk back to A-Frame position and hold for another 10 seconds
Repeat 4-6 times
1- A-Frame Position
2- A-Frame Walk to Squat
3- A-Frame Walk to Squat 2
4- Finish in Squat
Thank You
Thank you for taking the time to read this post, we sincerely hope that you find it useful and can use it to implement some positive changes in your daily routines. Take your time and work at your own level but be persistent and try to slowly improve on your own baseline. Please download your own FREE Cheatsheet to keep and to help with you practice and share this post with anyone who could benefit. If you have any questions or comments please just ask we would love to hear from you. Stay healthy and move well.
Childs Pose
Real Life Stories: Recovering from a disc injury
Fiona Callan is a CrossFitter and Ultra-marathoner who injured her back in 2017. She had an MRI which confirmed an L5/S1 disc bulge with nerve root irritation. In this interview we discussed how she avoided surgery and returned to the things she loved doing best.
Hi Fiona, thank you for taking the time to share your experience with us. We know you've come a long way from a pretty bad back injury. Before we begin, tell us a bit about yourself! What type of work do you do and what's your sport/exercise/fitness background?
I work in the NHS, primarily an office based job. Preceding my injury I was also studying for an MSc so basically spent all day and night sitting at a desk.
I started running in 2008, mainly 5k and 10k distance on roads but I wasn’t very good and didn’t enjoy it so moved to trail and hill running instead when I started gradually to increase my distance. I met some really cool people to run with as well. In 2012, I was talked into a trip to Nepal by a friend but it wasn’t until around 4 weeks to go that I found out he had signed me up to an ultra marathon. I didn’t even know what that was! It was sheer determination that got me through that and I really caught the ultra marathon bug.
In 2014 I started CrossFit as I thought some strength and conditioning type training would help with my running and I had no idea what I was doing in a conventional gym. The coaching and set workout approach has really worked for me and made me use muscles I didn’t know I had.
So the big question, when and how did you injure your back? Was it after one incident or was it something that gradually built up and got worse? What were your symptoms (i.e. back pain? leg pain? numbness etc...)
To be honest I’ve always had a bit of a lower back niggle, probably postural, but thought it would just go away. It was definitely something I started to feel more when I started CrossFit as I really had to use my back and core more than I had been doing running. Slowly I noticed it had started to affect my running, I had pain in my right buttock that shot down my leg now and again and my leg generally felt heavy. If I left it a few days it would go away but it meant I couldn’t really run or CrossFit as much as I wanted to.
It started affecting my job as I couldn’t sit comfortably for any period of time. I was travelling by train to Edinburgh at least twice a week which became difficult. On one journey I had to get off the train and go back to Glasgow as I couldn’t face sitting for an hour.
Then during a workout involving a barbell I cried so much I had to admit that something wasn’t right.
My initial symptoms were primarily in my lower back, there was a build up of pressure around my stomach and back even when I bent over the sink to wash my face. I tried to keep active but really scaled back on what I was doing. I kept up my hill walking as this is an activity I love doing with my nephew – I used poles and made Ewan carry my bag as he’s the young one! I tried running but could only manage 1k before I felt my back stiffen.
One Saturday I went walking with Dad and Ewan in the Lake District. It was an amazing day. The hill wasn’t too hard; we took our time and enjoyed it. It was the shooting pain in my right leg that woke me up early on the Sunday morning. I tried to stand up but my leg just wouldn’t work. I limped to the bathroom hanging onto the wall and at that point I knew there was something seriously wrong. It sounds dramatic but I genuinely felt paralysed down that whole side of my lower body, first thoughts were ‘I’ll never run again!’ and panicked. My boyfriend called NHS24 and a nurse managed to calm me down and suggested I took paracetamol with ibuprofen and try find a comfortable position until a doctor could get to me. A few hours and one injection later the pain had dulled. He said it was my sciatic nerve; I should try to relax and spend less time sitting down!
What was the initial management i.e. what treatment did you seek?
I got an appointment with Jonny who did some needling on my lower back/ glutes and gave me some exercises to do. I am the most impatient person and after a week of exercises I didn’t feel any different so I saw another physio (sorry!) who basically told me the same thing and gave me the same exercises. I really was in denial about how serious it was. I spoke to coaches in the gym, chatted to other runners and did a lot of Googling but all the answers were the same.
It was the mental part I actually found the toughest to deal with. I have made so many friends through running and CrossFit and my social media is full of it too so I was always seeing and hearing about all these amazing runs and PBs. I just felt stuck and disconnected. I saw my GP as I really felt like I was struggling to cope. People were always asking how I am and telling me I should ‘do this and do that’ and eventually I just got fed up talking about it. My GP didn’t really help me; she referred me to her physio friend but I didn’t go.
At the same time, Jonny had passed me onto Mariam for Clinical Pilates and it was during my consultation that she suggested some short term medication for my nerve problem in my right leg. I went to another GP for this and as well as giving me the medication, he was really keen to get me back running and to the gym so he referred me for an MRI.
Am I right in saying you ended up seeing a consultant neurosurgeon? What did the MRI show?
Yeah I was really lucky in that I got an MRI pretty quickly. I think the 2nd GP had something to do with that. A few weeks after the scan. I received a letter with a hospital appointment but with no other information. Frustrating and worrying. I thought well there must be something not quite right and because of my problem with patience, I called the GP and asked him to give me a brief overview of the scan. He said he could see a disc bulge and I should continue doing my physio exercises until my appointment. I had just started with the Clinical Pilates class so I let Mariam know the issue and she tailored exercises for me until I found out more about the problem.
So there was the prospect of having surgery? How did that make you feel? Was this something on the cards or wanting to avoid?
I remember getting a phone call from a surgeon in the spinal unit and it made me feel sick. I actually don’t remember what he said to me as the idea of back surgery just terrified me. I wasn’t exactly in crippling pain so the idea of surgery just felt a bit extreme to me. This was something I definitely wanted to avoid. I just really trusted my physios and they really believed I could get better without it. I didn’t feel that my pain was bad enough for surgery – for me this was the last resort, I’ve never heard positive stories about it.
At the appointment, the doctor went through my scan which I found fascinating. I actually felt a bit of weight come off my shoulders when I could physically see the issue. It had been hard to accept when I didn’t know for sure what the problem was but there it was clear in front of me. She then told me that they would do surgical intervention if I was getting sharp pains down the top of my leg. I told her I had that a few weeks before but it had been getting much better. We left it at that and I was told to get in touch if anything changed.
I had so many conversations with my boyfriend, my parents (and myself) and decided that it wasn’t the end of the world if I couldn’t run 50 miles or couldn’t deadlift 100kg as long as I could stay active. I would just scale back what I was doing.
You've spent the best part of a year doing some serious rehab with Clinical Pilates. In your own words can you explain what that is and how it helped you?
I had done a bit of Pilates before as I’d read and heard it was good for runners. It was one of those things I struggled to stick to because I never left the class feeling like I’d worked hard and my issue with patience didn’t help. When I told my boyfriend about it he signed me up for 6 weeks because he knew I’d have to go if he paid for it! I noticed a huge difference after these 6 weeks.
It is basically pilates but physio led so your exercises are all tailored to whatever issue you may have so we’re all doing something different generally. It’s a small class but everyone is in the same boat and really friendly. Mariam checks in with you regularly during the class and pushes you when you’re ready but also changing exercises if something isn’t quite feeling good.
I expected my exercises to all be lower back focused as that’s where my injury was but actually they’ve been full body movements. As well as having a stronger back, I have a stronger core and much improved posture. Mariam also spent some time working on my legs, particularly my right leg as the nerve had been affected and I had limited movement and very little strength.
Eventually you returned to CrossFit and trail-running. How long did that take from when you first injured yourself?
I was always doing a scaled back version of CrossFit and a bit of trail running while I was injured but I was mindful of undoing my hard work. It was important to me mentally that I kept in touch with coaches/ friends in the gym and my runner friends.
I accepted my injury in May 2017 and started Clinical Pilates in the October. In May 2018 I was a more confident runner so decided to train for a race following a plan, building up in distance and I finished the Mad Hatters Half Marathon and the Glentress Half Marathon with a PB and no back or leg pain. Not quite back at ultra marathon distance but I’m actually enjoying the shorter runs at the moment. In June 2018 I started back at CrossFit and noticed that I’m better at a lot of the movements as I actually use my back and core as I should. I’m always conscious of loading too much weight on bars and I know certain movements still aggravate my back but I know when to stop and I just need to gradually build my strength back up. I was asked if I’d like to be part of a team from the gym for a CrossFit competition, I said yes why not I can try and we finished in 3rd place with no back injury!
Most people in this day and age are seeking the "quick-fix" or miracle cure. In fact, most people in your shoes would opt for surgery given the opportunity. What advice would you give them?
Your back is such a major part of your body so decisions on surgery should never be made lightly. Unless a professional is telling you there is no other option I would encourage people to commit to the exercises, spend less time sitting down and stay active by doing anything you find fun (that’s obviously not going to hurt you)
Working through this injury has taught me so much about my body and my lifestyle as well as making me a better runner and CrossFitter. This is all coming from the most impatient person!
The Tool of our Trade
A revolutionary treatment technique used in physiotherapy is the use of an instrument or a tool, which enables the physiotherapist to locate and treat an area of soft tissue dysfunction. The official term is called Instrument Assisted Soft Tissue Mobilisation or IASTM.
IASTM - What is it?
A revolutionary treatment technique used in physiotherapy is the use of an instrument or a tool, which enables the physiotherapist to locate and treat an area of soft tissue dysfunction.
The official term is called Instrument Assisted Soft Tissue Mobilisation or IASTM. The technique itself is said to have evolved from the traditional Chinese Medicine technique called Gua Sha. However, Gua Sha uses the principle of Meridians to move the bad “Qi” out of the body. You could perhaps say that IASTM is a modernised version of Gua Sha using anatomical reasoning. IASTM is growing rapidly in popularity due to its effectiveness and efficiency in treating musculoskeletal conditions while remaining non-invasive compared to other treatment techniques such as Trigger Point Dry-Needling or Acupuncture.
IASTM is performed using an ergonomically designed tool most commonly made of stainless steel. The tool is used to detect and treat fascial restrictions, effectively treat scar tissue, chronic inflammation and/or degeneration. As with any physiotherapy treatment, the use of IASTM is also supplemented with exercise prescription and additional methods such as joint mobilisation designed to correct any biomechanical issues by addressing musculoskeletal strength and muscle imbalances or weaknesses.
IASTM Tooling around the knee at Physio Effect
How Does IASTM Work?
Soft tissue injury involves damage to muscles, ligaments, tendons and fascia (connective tissue) somewhere in the body. Common soft tissue injuries usually happen after a sprain, strain or a blow to the body resulting in ruptured blood vessels or overuse of a particular body part. Soft tissue injuries can result in pain, swelling, bruising and loss of function. Adhesions within the tissue may develop as a result of repetitive strain/overuse, surgery, or immobilisation.
Often, people with soft-tissue injuries do not seek out treatment until the injuries have become chronic (weeks/months after injury). By this point, the body has completed most of its self-healing process. Scar tissue and adhesions are formed during this healing process, which limits motion and often causes pain. Scar tissue and adhesions essentially act like super glue in your body. When scar tissue is created after injury, new cells are laid down excessively and in a disorganised manner. Scar tissue/adhesions prevent the muscle or other tissues from lengthening appropriately. It is often necessary to restart the healing process in order to remodel the soft tissues in the affected area. By introducing controlled micro-trauma to affected soft tissue using IASTM, a local inflammatory response is stimulated. This micro-trauma initiates reabsorption of inappropriate or excessive scar tissue and facilitates a remodelling of the affected soft-tissue structures. After IASTM treatment, scar tissue can be remodelled so that the cells become organised in a direction that better promotes movement.
The ergonomic design of the tool used for IASTM provides the physiotherapist with the ability to locate these soft tissue restrictions and allows them to treat the affected area with the appropriate amount of pressure.
What should I expect after an IASTM treatment?
It is important to note that IASTM’s ability to reinitiate healing comes from the fact that it is essentially re-injuring the body (although to a lesser degree and in a controlled manner). This may cause mild discomfort during the procedure. There may be soreness in the treatment area for a day or two following treatment and occasionally bruising may occur.
What are common conditions treated with IASTM?
Tennis or Golfer’s Elbow
Neck or Back Pain
Plantar Fascitis
Rotator Cuff , Achilles or Patella Tendinopathy
DeQuervain’s Tensosynovitis
Post-Surgical Scars
Ligament Sprains
Muscle Strains
IT Band Syndrome
Shin Splints
Chronic Ankle Sprains/Stiff Ankle
Arthritic Pain
What are the benefits following IASTM?
Improved range of motion
Improved muscle strength and function
Altered pain perception and reduction of pain
IASTM is a common treatment technique utilised by the therapists at Physio Effect. The dedicated team at Physio Effect provides a full package of services that will ensure you’re supported through injury prevention, assessment, recovery and helping you achieve your ultimate performance goals.
Dry Needling: The most effective pain treatment you may never have heard of!
Dry needling is a type of acupuncture that has become very popular with physiotherapists in recent years in our treatment of injury and pain.
Dry needling is a type of acupuncture that has become very popular with physiotherapists in recent years in our treatment of injury and pain. Also known as Western Medical Acupuncture, Dry Needling differentiates itself from traditional acupuncture by being administered to soft tissue structures such as muscles and fascia (connective tissue) in order to stimulate the central and peripheral nervous systems. This results in the release of pain relieving substances within the body, which can desensitise painful structures as well as the loosening of excessively tight muscles, therefore restoring movement and function and facilitating a healing response. Dry needling is often used in conjunction with other treatment techniques as part of a treatment plan. This is different from traditional Chinese Medicine type Acupuncture which places needles along meridian lines and is based on a model of treating and restoring energy flow within the body.
Why is it called Dry Needling and how does it work?
This was to differentiate it from the more traditional western medicine approach to treating painful muscles and joints that involved the use of a hypodermic needle to inject a medication such as a steroid solution.
Dry needling uses only a thin acupuncture-type needle to stimulate and deactivate myofascial trigger points, muscles and connective tissues. This can also have both diagnostic and treatment benefits whenever a practitioner is attempting to address problems in deeper muscles and structures that massage techniques cannot be effective at reaching.
Myofascial Trigger Points can be found to be causing pain in nearly every musculoskeletal pain problem. (Myo=Muscle; Fascia=Connective tissue - the term ‘myofascia’ describes that area). These trigger points present as hypersensitive localised muscle tenderness that can also cause prolonged ache in a more widespread area. They can arise from overloading and overuse of muscles and structures such as in sport or after trauma, or even while sitting with a poor posture with the example being pain to the neck or back. As well as pain, myofascial trigger points can cause weakness of the affected muscles and restrict range of movement, both which can contribute to other problems and compensations developing.
Generally as the needles used are so thin, a patient can often not even feel the needle being inserted. When dry needling is administered effectively to a myofascial trigger point the patient may experience a local twitch response from the muscle. This instantaneous involuntary contraction confirms the presence of a myofascial trigger point and the practitioner may stimulate this twitch response a number more times manually using the needle or via an electrical current from a TENS machine to successfully deactivate.
Results can often be instantaneous when assessing restricted ranges of movement in muscles and joints and your practitioner will often demonstrate this with before and after treatment testing.
After a dry needling treatment a patient may instantly experience improvement in their pain and dysfunction being treated however it is quite common to experience muscle soreness around the needle site for between 24-48 hours. This post treatment soreness, however, is comparable to what can be expected from most hands-on therapies such as deep tissue massage.
As dry needling is administered in a clinical environment by highly trained and regulated physiotherapists, it should be considered to be a very safe treatment option and your clinician will have taken every precaution to minimise risk of injury or infection from the needle. It would however not be advisable to try for anyone who suffers from a significant phobia of needles.
Injuries and conditions to consider dry needling with:
Postural and work-related pain
Sports injuries affecting all muscles and joints
Muscle and Joint Tightness
Disc injuries
Migraines and Tension-Type Headaches
Tendon Injuries
Fibromyalgia and Complex Regional Pain Syndrome
Back Strengthening Exercises for Desk-Based Workers
Let one of our Physios, Danny Wray, take you through a set of exercises which will help to strengthen your back and hips and that help counteract the negative effects of sitting.
At Physio Effect we routinely treat the general population for injuries and pain which can be attributed to a sedentary lifestyle. We have previously discussed the risks posed by excessive hours of sitting and how this is reaching almost epidemic levels in the Western world. Today's article provides some general exercise recommendations that can go some way to reducing this risk and counteracting the negative effects of sitting.
In an ideal world, those of us who have sedentary or sitting based occupations should aim to move, stretch, and be active for at least 1-2 minutes of every hour. While some of the exercises shown here may not be suitable for your particular work environment, any effort to perform a routine of this nature for 5-10 minutes before or after work or during a lunch break would go a long way to reducing the risk of pain and injury. General exercise and safe varied movement of any kind is also highly recommended.
Exercise 1 - Thoracic Rotation
Thoracic Rotation Start
Start on all fours with one hand placed behind your head.
Slowly turn the elbow towards the ceiling allowing your trunk to rotate and stretch
Hold at top position for 3-5 seconds. Repeat x 10 with each arm
Thoracic Rotation Finish
Exercise 2 - Dart
Dart - Start Position
Lay face down with thin pillow or folded towel for head support
Arms by your side, gently stretch your fingertips away from your shoulders allowing your shoulder blades to glide downward and slightly inward
Palms facing your hips, have your arms floating just off your side and not touching the floor
Keeping the back of your neck long and eyes looking to the floor, gently lift your head and upper body just off the floor - imagine lifting from your breast bone
Hold the finish position 3-5 seconds. Repeat 10 times 1-2 sets
Dart - Finish Position
Dart - Finish - Detail
Exercise 3 - Hip Flexor Stretch
Hip Flexor Stretch Start Position
Take a kneeling / lunge position as shown - use support of wall or furniture for balance if required
On the kneeling side gently engage your buttock and lower abdominal muscles - imagine you are tucking your tailbone in between your legs
You should feel a stretch at the front of your hip/ thigh. If balance allows gently raise the arm on the same side as the kneeling knee.
Hold the stretch for 30 seconds minimum and repeat 2-3 times each side.
Hip Flexor Stretch Finish Position
Exercise 4 - Cobra
Cobra Start Position
Lay face down with hands palms down about shoulder height
Using your arms slowly press out peeling your upper body slowly off the floor
Remain heavy in your hips trying to keep them in contact with the floor - relax your buttock muscles
Hold the finish position for 5-10 seconds, return to the start and repeat 5-10 times
Cobra Finish Position
Exercise 5 - Shoulder Bridge
Shoulder Bridge Start Position
Lay flat on your back with feet shoulder width apart and knees bent
Using your lower abdominals gently tilt your pelvis to press your lower back flat to the floor
Pressing through your heels, using your buttock and abdominal muscles gently peel your spine up from the floor starting with your tail bone.
Finish with your weight resting across your shoulder blades and your shoulders, hips and knees in a diagonal line
Hold finish position for 3-5 seconds, return to start and repeat 10 times for 2-3 sets.
Shoulder Bridge Finish Position
Exercise 6 - Superman
Superman Start Position
Start in all fours position with knees under hips, hands under shoulders and spine relaxed
Slowly extend out opposite arm and leg pointing the toes behind and the fingertips to the front
Keep gentle tension in your lower abdominals - think about drawing your bellybutton in towards your spine
Try to maintain spinal position throughout the movement, return slowly to start position
Repeat with opposite arm and leg, try 10-12 repetitions for 2-3 sets.
Superman Finish Position
Exercise 7 - Thoracic Extension with Foam Roller
Thoracic Extension with Foam Roller Start Position
Lying on your back with knees bent and feet flat, place a foam roller under your mid-upper back as shown
Take a deep breath in and then, as you exhale, slowly extend back over the roller to stretch your back. Try to keep your lower abdominals engaged to avoid over-arching your lower back
Support your head with your hands and be careful to stay relaxed in your neck. If you find this too intense or uncomfortable, try using a pillow or pillows to rest back onto
Hold the finish position for 2-3 breath cycles, return to start position and repeat 5 times
Move the roller to another position in your mid-upper back and repeat the process, aim to work on 3-5 positions along your spine
Thoracic Extension with Foam Roller Finish Position
Thoracic Extension with Foam Roller Alternate Finish Position
Exercise 8 - Pec Stretch
Pec Stretch Start Position
Stand as shown with arm at approximately shoulder height and palm to forearm placed against the doorframe
Slowly turn your body away by stepping your feet around to open and stretch the front of your chest and shoulder
Lean gently into the stretch, keeping your neck relaxed, hold for 30 seconds+, repeat x 2 on each side
Alternatively, use a doorway to position both arms in the stretch position, step forward to feel the chest and shoulder open and stretch. Hold 30 seconds+, repeat x 2.
Double Pec Stretch Position
While these are general exercise recommendations suitable for the majority of the population they are not prescriptive for any specific pain or injury. These exercises should be performed slowly and gently in a range of movement suited to your own level of ability and flexibility. The exercises should not cause any pain and we recommend that if you are in any doubt or if you are suffering from spinal or joint pain issues you should consult a healthcare professional for advice.
At Physio Effect we provide a wide range of services allowing us to not only treat your pain or injury but ensure that you are given the best advice specific to your individual needs to prevent your problem from recurring.
#KnowledgeShare – Back Mobility
It’s back month here at Physio Effect Glasgow - how to use a foam roller to help with back pain
17th March 2017
It’s Back Month here at Physio Effect! Here’s Jonny (and Ash) showing us how to use the foam roller for a bit of mobilisation!