Early Postpartum Tips for Pelvic Floor
Women’s health expert Physiotherapist Jenny Devlin gives insight on what you might expect from your postpartum body and the best approach to begin exercise and optimise your recovery
WRITTEN BY JENNY DEVLIN, MSK PHYSIOTHERAPIST AND SPECIALIST WOMEN’S HEALTH PHYSIOTHERAPIST AT PHYSIO EFFECT
So, you’ve just had a baby… CONGRATULATIONS!!
The first days and weeks postpartum can be a blur and prioritizing pelvic floor exercises might not be at the forefront of everyone’s mind. There are some things you can do, however, throughout the day to start working on your pelvic floor while also enjoying sweet baby cuddles.
BREATHE
Something that we do every day but often don’t do well. Once we have had a baby our breathing is often altered as our baby has been taking up the space in our abdominal cavity and achieving a deep breath might have been tricky for the past few months. Remembering how to take deep breaths can help with the healing process. Our diaphragm and pelvic floor move together and as a result breathing deeply in can help relax and lengthen the pelvic floor muscles and conversely exhaling can help engage the same muscles.
Getting the muscle pump of the pelvic floor working can aid pelvic congestion and help heal the tissues through lymphatic drainage.
Deep breathing can also help us enter into ‘rest and digest’ mode which can help us feel calm and decrease anxiety and enjoy being present with our baby.
You can practice breathing anywhere but it might be easiest sitting or in a semi-reclined position. Make sure you’re comfortable. Inhale slowly through the nose, feeling the air fill the lungs and the pelvic floor lengthen. Exhale gently through the mouth and feel the recoil of the tissues. Keep your shoulders and jaw relaxed. You can learn more about the structures that make up your abdominal cannister, including your pelvic floor in our recent Blog Post.
Posture
Throughout the day, check in with your posture while sitting, standing and moving around. Has your posture changed since having your baby? Can you find your way back to your previous position?
How we hold ourselves while feeding baby for many hours per day is important. Make sure baby is supported to come up to you, so that you don’t have to hunch over to feed. Try to maintain an upright posture for feeding as much as you can - it has an impact, not only on your back, neck and shoulders, but on your pelvic floor too! This NHS guide has ideas alternative breastfeeding positions from the commonly adopted ‘Cradle Hold.’
Have a think when you’re holding baby, are you always holding them on one side? Can you switch? Can you wear them for a while in a carrier instead of carrying them? Try placing your hands on your ribs and stacking them over your pelvis.
There are lots of little ways we can improve postures throughout the day to make our pelvic floor a little happier and function better too!
Pelvic Floor Exercises
Throughout the day try to practice a few pelvic floor muscle contractions. You may find it easier to do it lying down or in sitting. Check in with yourself and see what you can feel. You should be able to feel a gentle lift of the pelvic floor without your pelvis tilting and without your legs or bum muscles working hard. You should also be able to feel it relaxing. Try for some longer contractions and some short, fast ones too.
Women’s health Physiotherapist Mariam Kilpatrick demonstrating the ‘Butterfly’ Technique to connect with your pelvic floor.
Gentle Exercise
In the first days postpartum, take it easy. No matter how your baby was born, the body goes through a lot to bring your little one into the world. You might feel like you can do more exercise wise, but do you really need to? Give your body time to rest and recover and gradually build in your exercises. The first days or weeks might start out just thinking about pelvic floor, core and posture and progress from there. We are all about getting you back to doing the things you LOVE so let’s make sure you’re doing them sequentially in a way that’s right for your body and will allow you to continue doing them long term!
See a Pelvic Floor Physiotherapist
Pelvic floor symptoms are common, but they are not normal! We hear a lot of people normalizing pain or incontinence. Often ladies don’t know there is help out there but there is level 1, grade A evidence to show that pelvic floor assessment and treatment can improve pelvic floor function. Enjoy baby cuddles and gentle progressive exercises and anywhere from the 6 week mark, come and see us and have a pelvic floor evaluation so we can do an assessment, assist with any symptoms and help you work towards your goals, no matter what they are.
The Core
Think your core muscles are just a ‘six pack?’ You’re wrong! Learn more about your core and it’s importance in movement.
Written by Jenny Devlin, MSK Physiotherapist and Specialist Women’s Health Physiotherapist at Physio Effect
The Core
What do you think of when you hear the word ‘core’?
For most people, they think of the rectus abdominis muscles, or the “six pack muscles”, but the core is so much more than that!
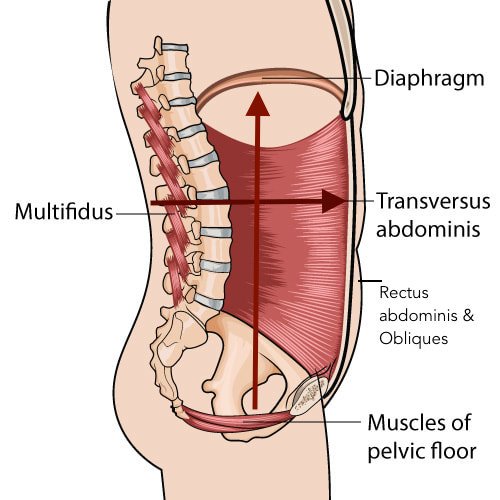
The core is actually a full canister that comprises a top, bottom, front and back. Respectively, these are:
The diaphragm
The pelvic floor
The transversus abdominis (deep stomach muscles)
The multifidus (deep back muscles)
Abdominal canister illustration courtesy of ‘The Wellness Blog for Women.’
These muscles work all the time to hold us upright and provide a base from which other muscles can operate. People will often tell us they ‘have no core’ which simply can’t be true or they would be a floppy noodle! What they mean is that they have forgotten how to tune in to activate their core and the good news is that this can be trained.
Our core canister houses our fluid and organs and is responsible for controlling pressure within the system, namely intra-abdominal pressure (IAP). IAP helps our ribs and spine stay in place and is the central mechanism from which we produce strength and stability. Since the muscles surround the canister, they are in prime position to help to control the pressure. IAP changes to match the task we are looking to perform and without a strong inner unit, it is challenging to keep our bodies moving and functioning effectively.
At Physio Effect we can offer you a path back to exercise safely after pregnancy.
Why do i have weakness in my core?
There are many things which can contribute to the core functioning less optimally - it could be the way you train or perform your sport, from being overweight or just a lack of body awareness of how to engage the correct muscles. In particular, pregnancy can lead to dysfunction as the muscles have been stretched out over nine months to accommodate the baby and then afterwards we often just hope they will go back to doing what they did before. Strength and coordination often need to be retrained and, while traditional abdominal exercises are great, it is important to ensure we have the deep core muscles working efficiently before we layer on the larger muscle groups. When we don’t have good core control, it can lead to injuries anywhere in the body such as the low back or the shoulder.
It is normal to have a diastasis rectus abdominus (abdominal separation) following pregnancy but when the pressure is not well controlled, we see doming at the linea alba (midline connective tissue). If we can work to control the IAP with the core muscles, we can minimise this doming and increase overall strength and performance since we are not losing pressure at our core canister.
Illustration of Abdominal Separation courtesy of Cleveland Clinic.
What can I do to strengthen my core?
It is important to spend time connecting to the core and learning how to coordinate the breath, pelvic floor and deep abdominal and low back muscles before adding more challenging exercises to your program. Our physiotherapists can provide you with some targeted core exercises that are specific to your needs. You could also consider our Clinical Pilates, Pregnancy Pilates or Postpartum Pilates Classes to strengthen your core.
To find out more, give us a call or book in online.
Pelvic Organ Prolapse
Pelvic Organ Prolapse - Signs, Symptoms and Treatment
PELVIC ORGAN PROLAPSE
WRITTEN BY JENNY DEVLIN, MSK PHYSIOTHERAPIST AND SPECIALIST WOMEN’S HEALTH PHYSIOTHERAPIST AT PHYSIO EFFECT. MCSP & HCPC
For a lot of people a diagnosis of, or even the thought of, pelvic organ prolapse is terrifying. It is extremely common though with the Royal College of Obstetricians & Gynaecologists suggesting that as many as 1 in 10 women over the age of 50 are affected. This number may well be higher with an increasing risk of complications after pregnancy and childbirth.
The good news is that many people are able to reduce or resolve their prolapse with the help of a pelvic floor physiotherapist. In this blog we explain more about Pelvic organ prolapse and look at how our experienced and specially trained Pelvic health Physiotherapists can help you.
What is pelvic organ prolapse (POP)?
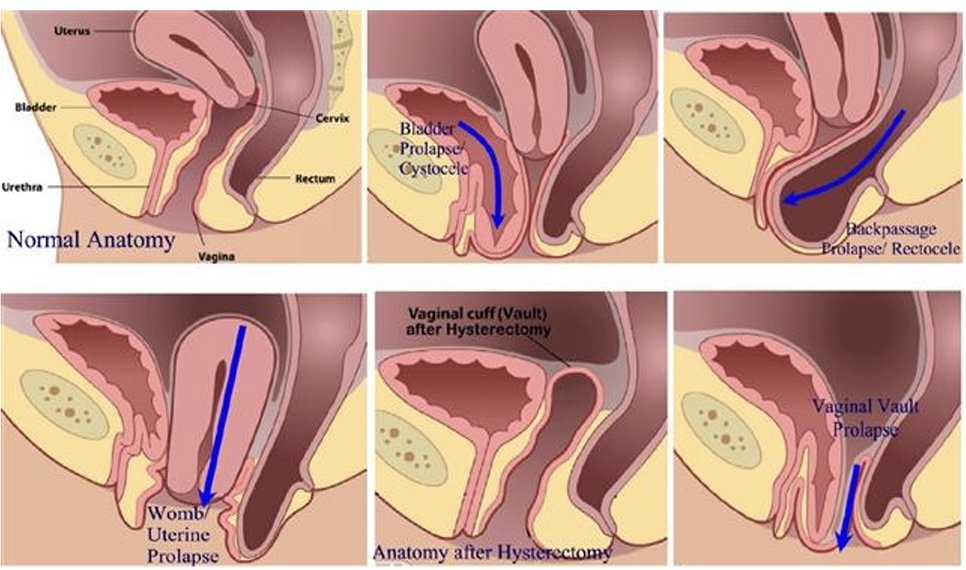
A pelvic organ prolapse occurs when a pelvic organ (or organs) bulge into the vaginal space. Strained, tight or weak muscles, ligaments or fascia can contribute to this. It can occur in different ways and we name the POP based on the organ that is not in its optimal position. A bladder prolapse (or cystocele) is where the bladder pushes against the front wall of the vagina. A uterine prolapse is where the uterus drops down into the middle of the vaginal space and a rectocele is when the rectum moves into the space at the back of the vaginal canal. You can also have a vaginal vault prolapse which occurs after a hysterectomy.
Pelvic Organ Prolapse
Symptoms of a pelvic organ prolapse
Prolapse affects everyone in a very unique way both physically and mentally. Some people live with prolapse and do not experience any symptoms. Other people can experience any number of symptoms which can be mild or affect your quality of life. Symptoms include:
pressure or heaviness in your pelvis area, which is often worse at the end of the day or with exercise
low back pain
urinary symptoms such as a slower stream, increased frequency or urgency to void, feeling of incomplete emptying of the bladder, urinary incontinence
bowel problems such as constipation, straining, feeling like the bowel doesn’t empty completely, increased frequency of bowel movements, faecal smearing (stool on the tissue after wiping clean), incontinence of faeces
Discomfort during sexual intercourse
Treatment options for pelvic organ prolapse
Pelvic Health Physiotherapy Assessment
Great news! Pelvic floor physiotherapy may be able to help with your symptoms of POP. Our team can help suggest changes you can make to your day to day routine to manage pressure on the organs, help with toilet positions to aid more effective urination/defecation.
Our specially trained Physiotherapists can assess muscle tension in the pelvic floor and abdominal muscles and help you to release this. We can also assess the strength and endurance of the muscles and teach you how to improve this if need be.
Physio instructed strengthening
We can guide you on correct strength and endurance exercises to help support the pelvic organs and the pelvis itself. This can help you in everyday functions when straining or lifting and on safely returning to sport. We can also make individual suggestions for more comfortable positions for intercourse.
Pessary For Pelvic Organ Prolapse
At Physio Effect our specialist team can assess and fit a pessary. A pessary is a device you wear inside the vagina, intermittently or continuously, to help hold things in position while you do the things you love. Once it is in place, you don’t feel anything but it can provide instant relief from that heaviness or pressure and can help with symptoms of incontinence too.
Cube Pessaries
Best of all once fitted these pessaries are designed for self management so you are in complete control and can remove and fit the pessary as required. After assessment and discussing your individual symptoms and needs our physiotherapists can help you decide if surgery might be the best route for you if conservative therapy has not worked.
We are here to help so please ask us anything. Hopefully this information makes things seem a bit less overwhelming and gives you hope that your symptoms can be improved. Give us a call or book in online for a full assessment and personalised treatment plan.
What is Pelvic Floor Physiotherapy?
What is pelvic floor physiotherapy and how can our team help you get back to doing the things you love symptom free?
Written by Jenny Devlin, MSK Physiotherapist and Specialist Women’s Health Physiotherapist at Physio Effect. MCSP & HCPC
What is pelvic floor physiotherapy?
Pelvic floor physiotherapists are musculoskeletal physios who have undergone specialised training in assessing and treating conditions that affect the pelvic area. This can be from pregnancy, childbirth or surgery but it does not have to be!
Some pelvic floor issues that can be treated with pelvic floor physiotherapy include:
Urinary and faecal incontinence
Urinary urgency, retention, frequency
Diastasis rectus abdominus
Pain with bowel movements or urination
Pain in the vulvar area (vestibulodynia, vulvodynia)
Painful intercourse (dyspareunia)
Constipation
Interstitial cystitis
Pudendal neuralgia
Endometriosis
Low back pain
Hip pain
Prenatal care - including pain management, exercise advice, positions for birthing, breathing techniques
Postpartum care - including return to sport
Jenny Devlin, specialist pelvic health Physiotherapist explaining pelvic health assessment
What does a pelvic floor assessment involve?
At your first appointment you will be asked several questions about your current symptoms, past symptoms and other relevant medical and social information.
We will then conduct a physical assessment which will be different for everyone depending on what’s going on with you. It will likely involve postural assessment, checking your pelvic alignment, tummy muscles and how your body moves when you do certain tasks like squat or stand on one leg.
If your pelvic floor seems to be involved then we will recommend an internal assessment. The benefits of a digital vaginal or rectal examination are that the physiotherapist is able to assess tension, strength, prolapse and improve activation of the muscles. The risks are that there may be local discomfort or emotional stress, skin reaction, nausea or bleeding, though we take all measures to minimise these risks.The alternative is doing an external examination and observing the abdomen and giving verbal cues for exercises, however, we will not know exactly what the muscles are doing and often progress is slower with this option. All of this will be discussed with your physiotherapist prior to therapy and throughout treatment. Consent to assessment and treatment can be withdrawn at any time. You are in charge!
Women’s Health Physiotherapist Jenny Devlin conducting a pelvic floor assessment with a female patient.
Does pelvic floor physiotherapy work??
Studies have shown that pelvic floor physiotherapy has Level 1, grade A evidence for treating urinary incontinence and pelvic organ prolapse. Clinical guidelines (2008) on the conservative management of urinary incontinence by the Society of Obstetricians and Gynaecologists of Canada recommend “proper performance of Kegel exercises should be confirmed by digital vaginal examination or biofeedback”. This is crucial because a high percentage of women can not contract their pelvic floor correctly. Further to that, performing more kegel exercises may not be what you need and an assessment with a trained pelvic floor physiotherapist can help guide you as to what treatment is most effective for your body.
Often people are prescribed pelvic floor physiotherapy in their postpartum period or when they are older but physiotherapy should be routine for pregnant people too. Research shows that pelvic floor muscle training between 20-36 weeks of pregnancy had a shorter second stage of labour, less urinary incontinence and less pregnancy related low back pain compared to people who did not perform pelvic floor exercises. This is an essential time to have your pelvic floor evaluated, learn optimal positions and breathing for labour and delivery and to set yourself up for a more successful postpartum recovery.
Make sure you align yourself with a pelvic floor physiotherapist who understands that not all pelvic pain is tissue based. Pain, especially chronic pain, is multifactorial and therefore it is so important that you find a physio who understands the relationship between pain, biological factors, the nervous system, psychological and social factors so that you can have the best outcome!
How do I know if pelvic floor physiotherapy is for me?
Do you have a pelvis? Then the answer is YES, pelvic physio is for you! Joking aside, there are so many reasons that might bring you to a pelvic physiotherapist. If you have pain or discomfort in your pelvis area; heaviness or pressure at the vulva, vagina or rectum; leaking of urine or stool; need to go to the toilet often or experience urgency or have pain with intercourse. If you have uncontrolled doming of your tummy muscles when you move or have noticed a gap between your tummy muscles. If you have issues with constipation, hip pain or low back pain. If you are pregnant and in pain, or are looking for exercise guidance or tips and tricks for labour and delivery. If you are postpartum (6 weeks after childbirth for a vaginal exam, though physiotherapy can start before that). If you want to make a plan for returning to running or working out or to make day to day tasks feel easier on your body.
Still can’t decide? Call us on 01412304766 to discuss or use the link below and book your initial assessment, we will figure out what is best for you.
Antenatal Pilates Classes at Physio Effect
Some exciting news! We have a NEW Antenatal Pilates class running in our studio within our Northside clinic at Borron Street. This physio-led Clinical Pilates class aims to prevent pregnancy related issues such as pelvic girdle pain (PGP), symphysis pubis dysfunction (SPD), posture related pain as well as a full body programme to prepare you for the birth of your child. During the class, you will be guided through an individualised programme relevant to your stage of pregnancy and any other issues discussed during your initial physiotherapy appointment.
WHEN: Wednesday evenings at 7PM from 21st October
**CLASS NOW FULLY BOOKED**
Please contact us below if you would like to be placed on our waiting list or if you wish to attend any of our other Clinical Pilates classes which will be a mixed group, but you will still be able to do an antenatal programme due to the bespoke nature of the class.
WHEN CAN I START?
As long as you have an uncomplicated pregnancy and your midwife/ doctor approves, you can begin from any time in your second trimester if you have no Pilates experience. If you have previous Pilates experience, you may begin earlier.
HOW DO I GET STARTED?
You will be required to have a 1:1 session with one of our physiotherapists before joining a class for the first time. During this appointment, your physiotherapist will be able to plan a bespoke Pilates programme for you based on your goals, requirements and stage of pregnancy. You will be introduced to the various Pilates props and equipment used during a class including the Pilates Reformer machine.
HOW MUCH DOES IT COST?
Antenatal Physiotherapy Appointment: £49
Single class rate: £25
6 classes: £120 (£20 per class)
12 classes: £220 (£18.3 per class)
You have flexibility to use the class blocks within the following time period:
● 10 weeks on a 6-class block
● 4 months on an 12-class block
WHAT HAPPENS IF I HAVE MY BABY BEFORE I USE UP ALL MY CLASSES?
You may use any remaining class credit towards our Crybaby Pilates Classes. This is our specialist Postnatal Pilates class which you may begin once you are at least 6 weeks postpartum after a non-complicated vaginal delivery or 8 weeks if you have had a C-section/assisted delivery with any complications.
CryBaby (Postnatal) Pilates Class
New Mummy Struggles: Exercise after Pregnancy
How one of our Physios managed getting back to fitness alongside the challenges of a new baby!
After giving birth to my first baby five months ago, life had changed as I knew it. Sleep deprivation… endless feeds… nappy changes… How does exercise fit into the picture?
I had always been a fit and active person, exercising 4-5x a week and continued to exercise right up until four days before my daughter was born. Before I knew it, I had this tiny human completely dependent on me. I felt like there was no time for anything else. Not long after I gave birth, we attended a family wedding. A family member commented that I had put on weight since having a baby and decided it was appropriate to tell me to stop eating junkfood. It was at this point I knew I had two choices: 1. Wallow in self-pity and never leave the house again 2. Find the motivation to do the things I enjoyed before having my baby. I chose the latter.
Since giving birth, I knew my body was no longer the same. I realised this after I came home from hospital and a 10-minute walk around the park felt like a marathon. As a physiotherapist who works with a lot of ante- and postnatal women, I am lucky to have the background knowledge on the human body after birth. I knew I couldn’t just jump back into what I was previously doing pre-baby. It was going to take time and patience. For the first six weeks, my exercise consisted of pelvic floor and abdominal exercises shown to me in hospital. This was all well and good when you are advised to do them every few hours, but when you’re dealing with a brand new baby; it’s the last thing on your mind! I therefore incorporated these exercises with a task I was doing constantly throughout the day - and that was feeding my baby (which was every 2-3 hours!) Every time I sat down to feed her, I made myself do them. I also went on daily walks with the buggy, which helped my mental wellbeing just to get outside the house.
After my 6-week check-up, I saw a physiotherapist who assessed my pelvic floor function and measured my belly for a diastasis recti; a condition that happens during pregnancy when the abdominal wall separates. This causes a small gap above or below the belly button. To address this, I attended mother and baby Pilates classes. Pilates focuses on the working relationships of the muscles around your trunk. These include your abdominals, diaphragm, pelvic floor and back muscles – ideal after having a baby! Being able to bring my baby along to the classes also made it easier for me not having to worry about a babysitter.
At 12-weeks, I felt I was ready to begin higher intensity exercise. After we put the baby to bed at night, I would go for a light jog for 15-20 minutes and gradually increased this as I felt comfortable. Thankfully having a baby in the spring meant long daylight hours for me to head out. I also joined a mother and baby bootcamp-style class, which incorporated strength and resistance exercises as well as high intensity interval training.
Common post-pregnancy myths that need to be debunked:
It’s normal to wee myself a little bit sometimes because I’ve had a baby
False: Incontinence post-birth is a sign of pelvic floor dysfunction and could indicate a prolapse. It is important to get this assessed by a women’s health physiotherapist to avoid long-term problems.
It’s normal to have back or pelvic pain because I’ve just had a baby
False: You may be in pain because of muscle imbalances and weaknesses. Seek advice from your physiotherapist for treatment and exercises to address any issues.
I’ve had a C-section so I don’t need to strengthen my pelvic floor
False: Your pelvic floor, regardless of how you gave birth, has been through a lot! It has carried the weight of your baby, the placenta and a 50% increase in blood volume for 9 months. This will greatly affect its ability to do its job properly compared to pre-pregnancy function.
Doing lots of ab-crunches and “planks” will help me get a flat tummy
False: These types of exercises should not be performed early on after birth as they cause excessive force on the abdominal wall, which may actually increase separation. It is best to strengthen the deeper abdominal muscles first with Pilates-type exercises.
It is important to remember that every woman is different. Exercise timescales are determined by your previous level of fitness, the type of birth you experienced and take into account any complications thereafter. Seek advice from your physiotherapist before commencing an exercise regime.
At Physio Effect we provide physiotherapy throughout your pregnancy journey and beyond. This includes ante- and postnatal assessment, treatment and physio-led Pilates classes. Our partners at Everyday Athlete Gym also run special mother and baby exercise classes.
Click here to see more about our ante- and postnatal services here at Physio Effect
One of our physios Mariam Kilpatrick with wonder-baby Aria